Key Points
-
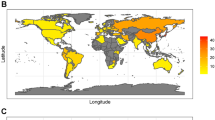
Helicobacter pylori persistently colonizes the gastric mucosa of humans, infecting approximately 50% of the population worldwide. The prevalence of H. pylori is decreasing in most parts of the developed world owing to improved sanitation, reduced transmission and the more frequent use of antibiotics in childhood.
-
Initial colonization of the hostile environment of the gastric mucosa by H. pylori requires specific adaptations, including flagellar motility, production of urease, chemotaxis and helical cell shape.
-
To establish persistent infection, H. pylori has evolved to avoid recognition by pattern recognition receptors of the innate immune system and to preferentially activate receptors coupled to anti-inflammatory signalling pathways. The pathogen-associated molecular patterns of this bacterium are substantially less biologically active than those of related Gram-negative enteropathogens.
-
Another H. pylori persistence strategy involves the prevention and manipulation of T cell-mediated adaptive immunity. Specific virulence factors are produced by all strains of H. pylori to block T cell activation, proliferation and effector functions, and to preferentially induce regulatory T cell responses rather than effector T cell responses. Asymptomatic carriers are more likely to preferentially generate TReg responses and harbour denser H. pylori populations than patients with peptic ulcer disease.
-
H. pylori causes gastric disease owing to its production of vacuolating cytotoxin and to a pathogenicity island-encoded type IV secretion system; both virulence determinants act together to promote the production of pro-inflammatory cytokines, to disrupt cell polarity and to cause tissue damage. The advantage of producing these virulence determinants for the bacterium remains poorly understood, but might involve improved iron acquisition or enhanced transmission.
-
As a consequence of the loss of H. pylori from Western societies, the incidence of peptic ulcer disease and gastric cancer has continuously decreased in the affected populations. At the same time, allergies and chronic inflammatory disorders have become more common; epidemiological and experimental evidence suggests an inverse causal association between the loss of H. pylori and the rise in these immunological disorders.
Abstract
The bacterial pathogen Helicobacter pylori has co-evolved with humans and colonizes approximately 50% of the human population, but only causes overt gastric disease in a subset of infected hosts. In this Review, we discuss the pathogenesis of H. pylori and the mechanisms it uses to promote persistent colonization of the gastric mucosa, with a focus on recent insights into the role of the virulence factors vacuolating cytotoxin (VacA), cytotoxin-associated gene A (CagA) and CagL. We also describe the immunobiology of H. pylori infection and highlight how this bacterium manipulates the innate and adaptive immune systems of the host to promote its own persistence.
Similar content being viewed by others
Main
Helicobacter pylori is a highly successful human pathogen that colonizes approximately 50% of the world's population. It is typically transmitted orally within families during early childhood and can persist for decades in its preferred niche, the gastric mucosa, despite triggering vigorous innate and adaptive immune responses. H. pylori infection causes chronic gastritis, which is asymptomatic in the majority of carriers but is considered a major risk factor for the development of gastric and duodenal ulcers and the gastric malignancies mucosa-associated lymphoid tissue lymphoma and gastric adenocarcinoma1. In addition to its association with cancer, H. pylori stands out from other Gram-negative bacterial pathogens in its ability to persist and establish chronic infection.
Contrary to long-held dogma, the stomach is not a sterile organ and is estimated to support a community of up to 200 bacterial species2. However, when H. pylori is present it is usually numerically dominant and is readily visible in gastric biopsy tissue sections as helical rod-shaped organisms covering the gastric epithelial cells and surrounding mucus. Initial colonization depends on bacterial urease activity and helical cell-shape modulation to penetrate the gastric mucus. Constitutive DNA and protein repair pathways, combined with bacterial genome diversification and attenuation of chemical radical production by the host cell, are now recognized as essential for persistence of the bacterium in this niche. The two known H. pylori toxins, vacuolating cytotoxin (VacA) and cytotoxin-associated gene A (CagA), have been the focus of attempts to understand H. pylori virulence. Although work on VacA has recently been reviewed3, we highlight new insights into functional interactions between VacA and CagA and the modulation of immune responses by VacA and another secreted virulence factor, the γ-glutamyl transpeptidase (GGT).
Besides its arsenal of virulence factors, persistence of H. pylori is strongly influenced by the ability of the bacterium to evade, subvert and manipulate the host's immune system. This bacterium can evade detection by several innate immune receptors through target modification and it can subvert other innate recognition pathways through the suppression of downstream signal transduction, whereas evasion of adaptive immunity is achieved by the modulation of effector T cell functions. In this Review, we discuss the remarkable ability of H. pylori to colonize and persist in the hostile environment of the human stomach through the interplay of several secreted virulence factors and the sophisticated manipulation of both innate and adaptive immune responses. We also highlight progress on understanding the consequences of persistence for both the bacterium and the host.
Colonization of the gastric mucosa
Escape from the acidic lumen. The stomach is a particularly challenging niche for bacterial habitation. In the lower bowel, which has a neutral or a slightly alkaline pH, bacterial density is highest in the lumen; by contrast, the production of gastric acid in the stomach, which results in a pH of 1–2, severely limits luminal colonization. Indeed, H. pylori can only survive for minutes in the stomach lumen and must quickly migrate to the gastric epithelial surface4. Similar to the intestine, the mucous layer in the stomach forms a physical barrier to bacterial penetration and probably acts as a scaffold for binding of the host's antimicrobial compounds5. Bacterial urease production is required for acid resistance through the localized production of ammonium ions, and flagellar motility allows penetration of the mucus6 (Fig. 1). Furthermore, urease activity facilitates flagellar motility through the mucous layer by changing the viscoelasticity properties of gastric mucins. At low pH, gastric mucins form a gel that effectively traps the bacteria, but urease-catalysed production of ammonium ions raises the pH to near neutral and the mucous gel transitions to a viscoelastic solution through which H. pylori can swim7,8. Regulators of motility, including chemotaxis9,10,11,12 and cell shape13,14,15, have been probed to discover additional colonization factors and to better define the optimal niche for H. pylori. Helical cell shape is thought to enhance motility through viscous media by a corkscrew mechanism, and cell shape mutants that have lost helical twist and/or curvature exhibit attenuated colonization13,14,15. Chemotaxis mutants have an altered localization, including lower numbers of bacteria that are in close association with gastric epithelial cells16 and that are deeply penetrating the gastric glands9. In addition to promoting clearance, the altered localization of chemotaxis mutants correlates with lower inflammation, impaired recruitment of CD4+ T cells and the absence of a T helper 17 (TH17) response10,16. Thus, the intimate association with the gastric epithelium promotes stable infection while simultaneously provoking more inflammation. Higher inflammation correlates with lower bacterial loads17, which suggests that H. pylori must actively manage its interaction with the host epithelium to avoid clearance and to persist at this site (Fig. 1).
During initial infection of the stomach lumen, urease-dependent ammonia production locally raises the pH, which promotes bacterial survival and solubilizes the mucous gel to facilitate bacterial motility. Chemotaxis (driven by pH and possibly other gradients) and helical rod shape promote flagellar motility away from the acidic lumen to the preferred niche of Helicobacter pylori, which is on and adjacent to gastric epithelial cells. SabA, BabA and other variably expressed adhesins might shift the balance from mucus-associated to cell-associated bacteria. Cell-associated bacteria alter gastric epithelial cell behaviour through vacuolating cytotoxin (VacA), cytotoxin-associated gene A (CagA) and CagL, which all have multiple cellular targets. CagL interactions with the α5β1 cell surface receptor are mediated through the RGD motif of the protein, whereas interactions with the other cell surface receptor (αvβ5 integrin) are RGD-independent. The combined action of these three effectors leads to a number of changes in the gastric epithelial cell, including CagA- and VacA-dependent disruption of cell polarity, which can promote iron acquisition and cell extrusion; CagA- and CagL-dependent induction of chemokines and/or the gastric hormone gastrin; CagL-dependent inhibition of acid secretion by the (H++K+)ATPase and cellular proliferation, apoptosis and differentiation, which are mediated by all three effectors. In addition to CagL, CagA and CagY (not shown) have been demonstrated to bind α5β1 integrins, although the precise interaction surface is unknown. PS, phosphatidylserine; T4SS, type IV secretion system.
Persistent colonization of the gastric mucosa. H. pylori uses diverse strategies to promote its survival despite robust immune responses. All H. pylori strains encode proteins that are important for detoxifying reactive oxygen species (ROS) — for example, catalase and superoxide dismutase — and H. pylori arginase limits nitric oxide production by macrophage-, neutrophil- and epithelial cell-derived nitric oxide synthase18,19. Moreover, multiple DNA repair pathways contribute to efficient colonization20 even while the surrounding host tissue accumulates DNA lesions21,22. Recent work has shown that H. pylori strains constitutively express DNA repair proteins such as RecA and therefore lack a classic SOS response to DNA damage23,24. Following DNA damage, H. pylori instead upregulates natural competence, which promotes chronic persistence, probably through enhanced genetic diversification23,25.
The H. pylori genome contains multiple intragenic and extragenic repeat sequences26. CagY, which is expressed on the cell surface and is required for the type IV secretion system (T4SS)-mediated translocation of the effector CagA (see below), can undergo recombination between internal repeat motifs that generally preserve the reading frame27. During experimental infection of mice and rhesus macaques, there is an accumulation of H. pylori CagY variants that have gained or lost T4SS activity. These results suggest that CagA translocation and the associated biological responses, including inflammation, can have both beneficial and detrimental effects on bacterial persistence, leading to selection for both retention and loss of T4SS activity28.
Among the 60 predicted outer-membrane proteins, the HOP family shares highly similar or identical sequences at their amino and carboxyl termini and includes several known or predicted H. pylori adhesins that promote binding to the gastric epithelium29. These shared sequences could promote intragenomic or intergenomic recombination. Sequencing of H. pylori HOP loci from human clinical strain collections has revealed probable gene conversion of the Lewis B binding adhesin gene babA with babB or babC30,31,32,33 and of sabB with the sialyl-Lewis binding adhesin sabA or omp27 (Refs 34, 35, 36). During experimental infection of rhesus macaques or mice with H. pylori, replacement of babA with babB produces strains that have lost the ability to bind immobilized Lewis B antigens32,37. Additionally, replacement of sabB with sabA leads to strains expressing two copies of sabA, which results in increased binding to sialyl-Lewis antigens on murine gastric tissues36. Some alleles of babA and sabA can undergo phase variation by slipped strand mispairing at dinucleotide sequences in the coding sequences or the homopolymeric tracts in their promoters, again leading to either loss of or elevated gene expression38,39,40. The carbohydrate antigens that are bound by these adhesins are expressed on the cell surface and/or on secreted glycoproteins such as mucin. Furthermore, some of these antigens, such as sialyl-Lewis antigens, are induced during inflammation. Phase variation by gene conversion and slipped strand mispairing leads to the development of subpopulations with variable adherence properties that could allow the pathogen to evade immune responses or resist shedding. This ability to generate diverse subpopulations might also affect transmission to new hosts.
Secreted toxins of H. pylori
VacA and CagA effectors. H. pylori strains actively manipulate host tissues and promote their own persistence through the activity of several secreted toxins, some of which are discussed below. VacA is a pore-forming toxin that disrupts cell polarity, promotes apoptosis of epithelial cells and inhibits T cell proliferation and effector functions3. The vacA gene is carried by all H. pylori strains, and sequence variation in several domains of its encoded protein is linked to varying expression levels and cell type-specific toxicity, as well as disease severity3. Another important toxin is CagA. Originally characterized as an immunodominant antigen from patients that are infected with highly virulent vacA alleles41,42, CagA is translocated into host cells by the Cag T4SS, which is encoded on the cagpathogenicity island (PAI)1,43. Strains that express CagA are associated with an increased risk of cancer, and transgenic expression of CagA in mice induces gastric carcinoma and other malignancies, which has led to its designation as a bacterial oncoprotein44.
CagA–VacA interactions. To function as an oncoprotein, CagA must persist in cells or act in a 'hit and run' manner. CagA is not readily detected in gastric cancer tissues45 and was therefore suggested to have a causative role only early in cancer progression. It has now been shown that translocated CagA is degraded by autophagy when the infecting strain has the m1 allele of VacA, owing to the ability of this VacA isoform to bind the cell surface receptor low-density lipoprotein receptor-related protein 1 (LRP1)46. VacA binding of LRP1 leads to a loss of reduced glutathione (GSH) in the cell and increased production of ROS. This in turn activates AKT kinase-dependent degradation of the tumour suppressor p53 and results in the induction of autophagy, leading to CagA degradation. Interestingly, autophagy is not activated in cells that express a variant form of the CD44 adhesion molecule46. These cells have increased intracellular levels of GSH owing to activation of xCT, a glutamate-cysteine transporter47, and therefore do not induce ROS or autophagy on VacA binding. CD44 is a cell surface marker that is associated with epithelial cancer stem cells and CagA can be detected in cells expressing variant-CD44 from patients with gastric cancer46. Paradoxically, tissue changes that are associated with H. pylori-induced gastric carcinogenesis, including the development of intestinal metaplasia, were thought to render the stomach less hospitable for H. pylori colonization, leading to lower colonization loads. However, H. pylori was shown to intimately interact with gastric progenitor cells in a mouse infection model48. This ability of H. pylori to colonize cells that have stem cell-like properties, and the persistence of CagA protein in these cells due to the activation of xCT, could provide a mechanism to account for a sustained role of H. pylori colonization and CagA in oncogenesis.
Once translocated into host cells, CagA can be tyrosine phosphorylated on EPIYA motifs49 by SRC and ABL family kinases. These two types of kinase are activated sequentially and in a tightly regulated manner, with SRC kinases mediating the initial, preferential phosphorylation of EPIYA-C (and EPIYA-D) motifs and ABL kinases phosphorylating any EPIYA motif later during the infection50. Phosphorylated CagA interacts with SHP2 tyrosine phosphatase and CSK kinase, whereas unphosphorylated CagA is known to interact with CRK adaptor, MET, growth factor receptor-bound protein 2 (GRB2), PAR1 (also known as MARK) and E-cadherin43. Collectively, these interactions lead to altered cell signalling and changes in cell polarity, extrusion, motility, proliferation and pro-inflammatory cytokine secretion1,43. As discussed below, many of these phenotypes have now been linked to the acquisition of nutrients by the bacterium to promote persistence and/or host pathology.
Under standard conditions, CagA expression is not required for stomach colonization, but it does promote inflammation in the Mongolian gerbil model51. Cag T4SS activity is often lost during murine infection, which complicates efforts to elucidate the pathophysiological roles of CagA during chronic H. pylori infection28,52,53. However, in a polarized cell culture model, CagA promotes increased basolateral uptake and transcytosis of transferrin, and VacA drives mislocalization of the transferrin receptor to sites of bacterial attachment to facilitate iron acquisition by the bacterium54. In cagA mutants, the formation of microcolonies on the apical surface of the cell requires iron supplementation, whereas this is not a requirement for wild-type bacteria, suggesting that CagA- and VacA-dependent cell polarity perturbations confer a nutritional benefit. Consistent with this hypothesis, CagA is required for efficient colonization of Mongolian gerbils under iron-limiting conditions54. Thus, CagA and VacA collaborate to promote efficient colonization in the iron-limited environment of the stomach and to moderate the pathological effects of CagA.
Ultrastructural insights into CagA secretion. Given the importance of CagA in persistence and pathology, there has been much interest in the mechanisms governing CagA delivery into host cells. Translocation of CagA from the bacterium to the host cell cytosol is mediated by the Cag T4SS. This is a contact-dependent secretion system that forms a large complex spanning the inner and outer membranes, which contains a pilus and several ATPases that promote T4SS assembly, pilus formation and CagA translocation55. The H. pylori Cag PAI encodes homologues or paralogues of the prototypical Agrobacterium tumefaciens Vir T4SS56, including the putative VirB7 (CagT), VirB9 (CagX) and VirB10 (CagY); inner- and outer-membrane-spanning channel subunits57; the major, VirB2 (CagC), and the minor, VirB5 (CagL), pilus subunits; and several additional H. pylori-specific Cag proteins that are required for CagA translocation (for example, CagH and CagI)58,59. Many Cag T4SS components have domain structures that are distinct from their Vir counterparts. For example, the VirB10 homologue CagY is considerably larger (∼220 kDa) and contains additional domains that are composed of repeat regions27. Additionally, transmission electron microscopy studies suggest that the three core cell envelope-spanning channel subunit homologues (CagY, CagT and CagX) localize to the pilus surface or to the base of the pilus60,61. A later study localized CagL and CagA to the tip of the pilus62. CagL was suggested to function as a tip adhesin that binds to α5β1 integrin (a host cell receptor for CagL) through an RGD motif and neighbouring sequences62,63 (Fig. 1). CagL binding and α5β1 integrin signalling were found to be required for both pilus extension and CagA translocation. Soluble RGD peptide could partially rescue the CagA translocation defect of a cagLRGA mutant, but not a ΔcagL deletion strain, suggesting a two-step model in which surface exposed CagL binds and activates α5β1 integrin, partially activating focal adhesion kinase (FAK) and SRC kinase, promoting pilus extension. In a second step, pilus-associated CagL further stimulates α5β1 integrin, in addition to stimulating the activities of FAK and SRC, thereby inducing CagA translocation and ensuring its rapid tyrosine phosphorylation by SRC.
The relationship between pilus formation and CagA secretion was further explored by field emission scanning electron microscopy, which readily detects Cag T4SS-dependent pili64. This technique confirmed the requirement of CagL for pilus formation and also revealed a hyperpiliated phenotype for cagH mutants, which, like cagL mutants, fail to translocate CagA64. One study showed that a ΔcagY mutant produces pili28, which is surprising because another study found that CagL is unstable in a ΔcagY mutant59. Currently, the mechanism by which CagL (or CagA, CagT, CagX and CagY) becomes surface exposed or incorporated into pili has not been explored. Collectively, these data suggest that pilus formation is not sufficient for CagA translocation, that pilus formation can proceed in the absence of at least one core T4SS component, and that there might be CagL-independent mechanisms of integrin activation, of pilus assembly and of CagA translocation in some strains. In fact, CagA, CagI and CagY were shown to bind α5β1 integrin in vitro and in yeast two-hybrid studies65. CagA, in particular, shows a much higher integrin-binding affinity in vitro than CagL; unlike CagL, CagA binding is not inhibited by the Yersinia entercolitica RGD-containing invasin, which would indicate that CagA and CagL use different integrin interaction surfaces. Antibodies that prevent integrin switching between a bent and an open configuration block CagA translocation65, and the α5β1 integrin interaction domain of CagA was shown to inhibit CagA translocation when provided as a soluble peptide66, indicating that a complex series of molecular interactions is required for integrin activation and CagA secretion. Further insights into the precise nature of the interactions between CagA, CagL and host interaction partners are beginning to be revealed by structural and molecular evolution studies (Box 1).
CagL effector functions. Although the CagA translocation defect of cagL mutants suggests that CagL has a structural role as part of the T4SS, a number of studies suggest additional functions67,68,69,70. Studies using purified recombinant CagL revealed that the protein can induce cell spreading and focal adhesion formation in a similar manner to the host extracellular matrix RGD-containing protein fibronectin69. CagL activates epidermal growth factor receptor (EGFR) more efficiently than fibronectin, and this was shown to result from RGD-dependent displacement of ADAM17 (disintegrin and metalloproteinase domain-containing protein 17) from α5β1 integrin, thus activating ADAM17 protease activity68. ADAM17 cleaves and releases surface-bound heparin-binding EGF-like growth factor. The resulting activation of EGFR in gastric epithelial cells represses (H++K+)ATPase activity (diminishing acid secretion) via a repressive nuclear factor-κB (NF-κB) binding site in the (H++K+)ATPase promoter. CagL also binds αvβ5 integrin independently of its RGD motif, which mediates the induction of gastrin70. Gastrin is a potent inducer of acid secretion, so simultaneous activation of gastrin and repression of the (H++K+)ATPase could explain the observed hypergastrinaemia and hypochlorhydria during chronic H. pylori infection. Finally, CagL RGD-dependent activation of α5β1 integrin activates the pro-inflammatory cytokine interleukin-8 (IL-8) independently of CagA translocation and nucleotide-binding oligomerization domain-containing 1 (NOD1) signalling67, indicating that CagL induces inflammation. An increased risk of cancer and ulcers, which is associated with the carriage of the Cag PAI, has mostly been attributed to CagA but these studies indicate that CagL may be an equally important effector. Furthermore, studies on the evolution of the Cag PAI suggest that additional Cag proteins can directly interact with host proteins through exposure on the cell surface or as novel effectors (Box 1).
Evasion of innate immune recognition
In addition to the multiple virulence factors that H. pylori uses to manipulate the host and ensure its persistence, the bacterium has evolved elaborate strategies to evade and subvert host immune defences, and these strategies are key to the success of this pathogen. The first defence barrier against H. pylori is the mucus produced by the epithelial cells lining the gastric mucosa and the innate immune cells that either reside in the gastric lamina propria under steady state conditions or are recruited there during infection. The detection of conserved pathogen-derived molecular structures (pathogen-associated molecular patterns (PAMPs)) by epithelial cells and innate immune cells occurs via four distinct classes of innate immune receptors (pattern recognition receptors (PRRs)) that differ in their subcellular localization, their coupling to downstream signalling pathways and their specificity. H. pylori avoids detection by several types of PRR that are crucial for the recognition of other Gram-negative enteropathogens.
Evasion and manipulation of TLR and RLR recognition. The best-defined among the four classes of PRR are the Toll-like receptors (TLRs). TLRs are either exposed on the surface of the plasma membrane or localized to endosomes, and they bind diverse classes of PAMPs. Among these are the ligands for TLR4 (lipopolysaccharide (LPS)), TLR2 (lipoteichoic acid and lipoproteins), TLR3 (double-stranded RNA and polyinosinic:polycytidylic acid), TLR5 (flagellin) and TLR9 (unmethylated CpG). H. pylori largely avoids recognition by TLRs, the best understood example of this being the evasion of TLR4 detection of LPS. H. pylori LPS is predominantly tetra-acylated and is 1,000-fold less biologically active than the hexa-acylated LPS of Escherichia coli71. Furthermore, the reduced biological activity of H. pylori LPS was recently shown to result from the removal of phosphate groups from the 1′- and 4′-positions of the lipid A backbone, which generates LPS that has less negative charge, resists binding by antimicrobial peptides (such as polymyxin B) and escapes detection by TLRs72. The phosphatases responsible for lipid A modification in H. pylori have been identified and the respective gene deletion mutants fail to colonize experimentally infected mice72. The TLR (or TLRs) involved in the residual detection of H. pylori LPS remain a matter of debate; whereas several studies using purified LPS have implicated the classical LPS sensor TLR4 (Refs 73, 74), other studies suggest that TLR2 is the main sensor of H. pylori LPS75,76 (Fig. 2). A clear interpretation of the published studies is complicated by the fact that they rely on models in which the respective TLR is ectopically expressed, often in the absence of its co-receptor, and the fact that both TLR4 and TLR2 participate in the detection of other non-LPS-related PAMPs of H. pylori77,78, which may contaminate LPS preparations.
Helicobacter pylori harbours pathogen-associated molecular patterns (PAMPs) that have evolved to evade detection by pro-inflammatory Toll-like receptors (TLRs). H. pylori expresses tetra-acylated lipopolysaccharide (LPS), which is less biologically active than the hexa-acylated form that is typical of other Gram-negative pathogens owing to specific lipid A modifications that prevent detection by TLR4. H. pylori flagella are not detected by TLR5 owing to mutations in the TLR5 binding site of flagellin. The DNA of the bacterium, as well as a currently uncharacterized PAMP (and possibly H. pylori LPS) are detected by TLR9 and TLR2, respectively; these TLRs predominantly activate anti-inflammatory signalling pathways and anti-inflammatory interleukin-10 (IL-10) expression. 5′ triphosphorylated RNA is detected by the RIG-like helicase receptor family (RLR) RIG-I, which activates the transcription factors IRF3 and IRF7 to induce type I interferon (IFN; IFNα and IFNβ) expression. Bacterial RNA is also potentially detected by TLR8 in endosomes. The fucosylated DC-SIGN ligands of H. pylori suppress activation of the signalling pathways downstream of this C-type lectin receptor (CLR) and activate anti-inflammatory genes. Please note that not all depicted TLRs, RLRs and CLRs are necessarily expressed by the same cell type; only one generic cell type is shown here for simplicity. CARD, caspase activation and recruitment domain; DC-SIGN, dendritic cell-specific intercellular adhesion molecule-3 grabbing non-integrin; DD, death domain; MYD88, myeloid differentiation primary response gene 88; NF-κB, nuclear factor-κB; TIR, Toll/interleukin-1 receptor domain.
Another putative H. pylori PAMP, flagellin, escapes recognition by TLR5 owing to modifications in the N-terminal TLR5 recognition domain79 (Fig. 2). Mutating residues 89–96 of Salmonella enterica subsp. enterica serovar Typhimurium flagellin to the corresponding flaA sequence of H. pylori abolishes its recognition by TLR5 (Ref. 80). Experiments using dendritic cells lacking TLR2, TLR4, TLR7 and TLR9, or combinations thereof, revealed that the innate immune system recognizes H. pylori nucleic acids77. Intracellular delivery of H. pylori DNA to dendritic cells by lipofection efficiently activates endosomally localized TLR9 (Ref. 77); however, the net effect of this activation is anti-inflammatory rather than pro-inflammatory81,82,83 (Fig. 2). TLR9 signalling has anti-inflammatory consequences in the early stages of infection in a mouse model81, and H. pylori DNA can even be used therapeutically to treat experimentally induced inflammatory bowel disease in mice82,83. The biological activity of H. pylori DNA may account for the inverse correlation between H. pylori colonization and the risk of developing inflammatory bowel diseases84, which has been attributed to a specific immunoregulatory sequence (TTTAGGG) that seems to be unique to the H. pylori genome82,83. H. pylori RNA sensing by dendritic cells has been suggested to be mediated by endosomally localized TLR8 (Ref. 77), as well as by a cytoplasmic nucleic acid sensor, RIG-I, which belongs to the RIG-like helicase receptor family (RLR). RIG-I seems to be required for the detection of 5′ triphosphorylated H. pylori RNA and the ensuing IRF3- and IRF7-dependent induction of type I interferons (IFNs) by dendritic cells77 (Fig. 2). It is currently unknown whether the activation of RIG-I and the H. pylori-induced production of type I IFNs has predominantly pro-inflammatory or anti-inflammatory effects.
The detection of H. pylori non-LPS ligands by TLR2 is another example of how H. pylori exploits the immune system for the induction of anti-inflammatory responses. Activation of TLR2 triggers the myeloid differentiation primary response gene 88 (MYD88)-dependent expression of several anti-inflammatory genes, most notably IL-10 (Ref. 77) (Fig. 2). Furthermore, Tlr2−/− micethat are infected with Helicobacter felis, a close relative of H. pylori, are better able to control experimental infections than wild-type mice and develop stronger T cell responses and T cell-driven immunopathology78. The effects of TLR2 gene deletion are phenocopied by Myd88−/− mice, indicating that the absence of anti-inflammatory signals induced by Helicobacter spp. is phenotypically dominant over the simultaneous lack of MYD88-dependent pro-inflammatory signals that are induced by other TLRs78.
Suppression of CLR-mediated signalling. In addition to its TLR and RLR ligands, H. pylori also harbours ligands for a third class of PRR, the C-type lectin receptors (CLRs). The best characterized of these are fucosylated ligands that bind to the CLR family member DC-SIGN85. In contrast to pathogens such as Mycobacterium tuberculosis and HIV, which express mannosylated DC-SIGN ligands and which activate pro-inflammatory downstream signalling pathways, the fucose residues of the DC-SIGN ligands of H. pylori actively dissociate the signalling complex downstream of DC-SIGN (consisting of the scaffold proteins LSP1, KSR1 and CNK and the kinase RAF1) and suppress pro-inflammatory signalling85 (Fig. 2). The differential biological effects of mannosylated and fucosylated DC-SIGN ligands are consistent with the proposed role of this PRR in tailoring and fine-tuning adaptive immunity to specific pathogens through the DC-SIGN- and RAF1-mediated acetylation of TLR-activated NF-κB86. Acetylation of the NF-κB subunit p65 both prolongs and increases IL-10 transcription to enhance anti-inflammatory cytokine responses86.
In summary, most of the available data support the conclusion that H. pylori avoids the induction of a strong pro-inflammatory response, as well as subsequent adaptive immunity and clearance, through two main mechanisms: the evasion of innate immune detection by pro-inflammatory TLRs and the preferential activation and manipulation of anti-inflammatory TLRs and CLRs. Together, these strategies promote the persistence of the organism.
Activation of NLRs and the inflammasome
The heterogeneous cytoplasmic family of NOD-like receptors (NLRs) comprise the fourth and final family of PRRs. NLRs detect a wide range of PAMPs and are essential for sensing host-derived damage-associated molecular patterns that are released following perturbations of tissue homeostasis87. Broadly speaking, NLRs fall into two categories: NOD1 and NOD2 recognize metabolites and activate the transcription factor NF-κB to induce innate and adaptive immune response genes88, whereas most other NLRs promote the assembly of multiprotein complexes called inflammasomes, which activate the cysteine protease caspase 1 (Ref. 89).
Detection of H. pylori peptidoglycan by NOD1. NOD1-mediated detection of H. pylori peptidoglycan was one of the first PRR-mediated innate immune pathways found to become activated on H. pylori infection90. Although initial work indicated that only T4SS-proficient H. pylori strains (harbouring a functional Cag T4SS) could deliver peptidoglycan and its active metabolite (meso-diaminopimelate-containing N-acetylglucosamine-N-acetylmuramic acid) into the cytoplasm of host epithelial cells90, it is now clear that outer-membrane vesicles (OMVs) from Cag PAI-negative strains of H. pylori can also target peptidoglycan to NOD1 (Ref. 91) (Fig. 3). Intragastric delivery of OMVs in mice induces innate and adaptive immune responses through a NOD1-dependent but TLR-independent mechanism91. The delivery of peptidoglycan by both OMVs and the T4SS occurs at cholesterol-rich lipid rafts91,92 (Fig. 3). In addition to the initially reported NOD1 signalling pathway resulting in NF-κB translocation to the nucleus90, NOD1 also activates the transcription factor AP1 via ERK- and p38-dependent pathways93. A direct consequence of NOD1 signalling is efficient killing of H. pylori by β-defensin 2, an antimicrobial peptide produced by NOD1-activated gastric epithelial cells94. The idea that H. pylori-induced activation of NF-κB depends on NOD1 has recently been challenged by a report showing that the introduction of a small interfering RNA (siRNA) specific for NOD1 does not alter the nuclear translocation of the NF-κB subunit p65 (Ref. 95). This new study provides evidence for an alternative NOD1-dependent signalling pathway, which activates the IRF3 and IRF7 transcription factors to induce the production of type I IFNs that are required for H. pylori-specific cytokine and chemokine responses, and infection control95 (Fig. 3).
Helicobacter pylori peptidoglycan is delivered to the cytoplasmic NOD-like receptor (NLR) NOD1 (nucleotide-binding oligomerization domain-containing 1) through either the type IV secretion system (T4SS; via its interaction with α5β1 integrin at cholesterol-rich lipid rafts) or through outer-membrane vesicles (OMVs). Activated NOD1 induces the AP1- and nuclear factor-κB (NF-κB)-dependent expression of pro-inflammatory cytokines and defensins and the IRF3- and IRF7-dependent expression of type I interferons (IFNs; IFNα and IFNβ). Additional unidentified H. pylori NLR ligands activate the inflammasome to induce cleavage of autoproteolytic pro-caspase 1 and the subsequent processing and release of mature interleukin-1β (IL-1β) and IL-18. IL-18 binds to its receptor on naive T cells and promotes FOXP3-dependent CD4+CD25+ regulatory T (TReg) cell differentiation and immune tolerance, which in turn prevents clearance and ensures persistent colonization of H. pylori. By contrast, IL-1β binding to its receptor induces T-box transcription factor (TBET)- or retinoid-related orphan receptor γt (RORγt)-dependent T helper 1 (TH1) and TH17 differentiation and the expression of the respective signature cytokines IFNγ and IL-17. Note that the pictured innate immune cell is a dendritic cell, whereas peptidoglycan-induced NOD1 signalling has been demonstrated in gastric epithelial cells. ASC, apoptosis-associated speck-like protein containing a CARD; CARD, caspase activation and recruitment domain; LRR, leucine-rich repeat domain; MAPK, mitogen-activated protein kinase; PAI, pathogenicity island; RICK, receptor-interacting serine/threonine kinase.
Inflammasome activation by H. pylori. H. pylori harbours one or more ligands that trigger activation of the inflammasome and of caspase 1, a cysteine protease that controls the processing and secretion of two cytokine precursors, pro-IL-1β and pro-IL-18 (Ref. 87). Like other caspases, caspase 1 is synthesized as an inactive precursor, which becomes auto-proteolytically activated only after inflammasome assembly. Inflammasome assembly in turn is regulated by ligand binding and subsequent hetero-oligomerization of inflammasome sensors in conjunction with an adaptor molecule, ASC (apoptosis-associated speck-like protein containing a caspase activation and recruitment domain (CARD)), and pro-caspase 1 (Refs 87, 89). Whereas the inflammasome ligands and NLR sensors that are involved in H. pylori detection remain obscure, in vitro and in vivo studies have demonstrated that caspase 1 becomes activated in dendritic cells following co-culture with H. pylori, and that IL-18 and IL-1β are processed and released into the infected gastric mucosa96,97 (Fig. 3).
There is no evidence to suggest that H. pylori actively avoids inflammasome or caspase 1 activation. In fact, mice lacking caspase 1 can clear an experimental infection with H. felis or H. pylori more efficiently than wild-type animals and have more pronounced pathogen-specific T cell responses and T cell-driven immunopathology96. The explanation for this unexpected observation was provided by mouse strains lacking either IL-18 or its receptor, IL-18R: these mice phenocopy the effects of caspase 1 gene deletion; that is, they clear the infection better than wild-type mice owing to enhanced T cell responses and, as a consequence, they develop more severe immunopathology96,98. Further analysis revealed that IL-18 is crucial for inducing CD4+CD25+FOXP3+regulatory T cell (TReg cell) responses to H. pylori (Fig. 3), which in turn restrict excessive effector T cell activation and promote persistence98. Interestingly, IL-1β (the other caspase 1 cytokine substrate) apparently opposes IL-18 function. Il1r−/− animals that lack the receptor for IL-1β fail to launch H. pylori-specific TH1 and TH17 responses, and cannot control an experimental infection (even when vaccinated against H. pylori before challenge) and, as a consequence, are protected against even the mildest forms of infection-associated immunopathology96. These data corroborate an earlier report showing that stomach-specific expression of human IL-1β is sufficient to induce gastric inflammation and gastric cancer in transgenic mice99, and they also explain why promoter polymorphisms that are associated with increased steady-state levels of IL-1β predispose carriers to a high risk of gastric cancer100. Furthermore, the effects of Il1r gene deletion seem to be phenocopied by H. pylori-infected mice lacking the inflammasome adaptor ASC101. In conclusion, detection of H. pylori by NLRs and subsequent activation of the inflammasome and downstream signalling pathways is crucial for efficient infection control (in the case of NOD1 signalling and inflammasome-mediated IL-1β secretion) and at the same time ensures the restriction of excessive T cell responses and immunopathological tissue damage (by inflammasome-mediated IL-18 secretion).
Modulation of effector T cell responses
Suppression of TH1- and TH17-mediated immunity. Experimental infection studies have highlighted the elements of the innate and adaptive immune systems that are required for the control of H. pylori infections, particularly for the generation of vaccine-induced protective immunity17,102,103,104,105,106,107. Whereas B cells and antibodies are dispensable for H. pylori control103,104,107 (at least for the suboptimal, non-sterilizing reduction in colonization by 1–2 orders of magnitude that is considered the gold standard in the H. pylori vaccinology field (Box 2)), it is now clear that CD4+ effector T cells (not to be confused with the CD4+ TReg cells mentioned above), and in particular TH1 and TH17-polarized effector T cell subsets and their signature cytokines, are crucial for the control of this infection17,102,106. The same T cell subtypes have been implicated in promoting the immunopathological changes of the chronically infected gastric mucosa that manifest histologically as atrophic gastritis, compensatory epithelial hyperplasia and intestinal metaplasia in experimentally infected animals and symptomatic human carriers108,109.
Two virulence factors have been specifically implicated in the manipulation and inhibition of human T cells (Fig. 4). VacA inhibits T cell proliferation by interfering with the T cell receptor–IL-2 signalling pathway at the level of the Ca2+/calmodulin-dependent phosphatase calcineurin110,111. VacA prevents nuclear translocation of the T cell transcription factor NFAT and its subsequent transactivation of T cell-specific immune response genes110,111 (Fig. 4). Further studies have since identified β2 integrin (CD18) as the receptor for VacA on human T cells112; β2 integrin associates with CD11a on T cells to form the heterodimeric transmembrane receptor LFA1 (lymphocyte function-associated antigen 1). H. pylori exploits the recycling of LFA1 to facilitate VacA uptake112 in a manner that depends on protein kinase C-mediated serine/threonine phosphorylation of the β2 integrin cytoplasmic tail113. The other H. pylori virulence determinant that is implicated in T cell inhibition is GGT114,115. Similar to VacA, GGT is a secreted factor that blocks the proliferation of T cells through a mechanism that involves the inhibition of cyclin-dependent kinase activity in the G1 phase of the cell cycle through the disruption of the RAS signalling pathway114,115 (Fig. 4).
All strains of Helicobacter pylori express the secreted virulence factors vacuolating cytotoxin (VacA) and GGT to directly inhibit T cell activation, proliferation and effector functions. Hexameric VacA binds to the β2 integrin subunit of the heterodimeric transmembrane receptor lymphocyte function-associated antigen 1 (LFA1); the receptor complex is internalized following protein kinase C (PKC)-mediated serine/threonine phosphorylation (P) of the β2 integrin cytoplasmic tail. Cytoplasmic VacA prevents nuclear translocation of NFAT by inhibiting its dephosphorylation by the Ca2+/calmodulin-dependent phosphatase calcineurin, and thereby blocks interleukin-2 (IL-2) production and subsequent T cell activation and proliferation. GGT arrests T cells in the G1 phase of the cell cycle, preventing their proliferation. Both VacA and GGT also indirectly prevent T cell immunity by re-programming dendritic cells (DCs); VacA- and GGT-exposed dendritic cells produce IL-10, and induce the FOXP3- and contact-dependent differentiation of T cells into CD4+CD25+FOXP3+ regulatory T (TReg) cells while simultaneously preventing T helper 1 (TH1) and TH17 differentiation. TReg cell differentiation further depends on dendritic cell-derived IL-18, which is processed upon activation of caspase 1, and binds to its receptor on naive T cells. Depicted interactions at the T cell–dendritic cell synapse include major histocompatibility complex class II (MHCII) binding to the T cell receptor (TCR) and binding of co-stimulatory molecules CD80 and CD86 to CD28. Dendritic cell-derived and/or TReg cell-derived IL-10 further suppresses TH1 and TH17 effector functions. Note that the direct effects of VacA on T cells seem to be specific to humans, whereas indirect effects of VacA and GGT on T cells through dendritic cells have only been documented in the murine system. CaM, calmodulin; CnA, calcineurin A; GGT, γ-glutamyl-transpeptidase; RORγt, retinoid-related orphan receptor γt; TBET, T-box transcription factor.
Skewing of T cell responses. Both VacA and GGT also affect T cell activity in an indirect manner by promoting the preferential differentiation of naive T cells into TReg cells116. TReg cell differentiation in response to H. pylori infection requires the direct interaction of naive T cells with 'tolerogenic' dendritic cells that have been exposed to H. pylori, either in the gastric mucosa or in the stomach-draining (gastric or mesenteric) lymph nodes98,117,118. Dendritic cells that have been exposed to H. pylori fail to induce effector T cell responses of the TH1 and TH17 type in vitro and in vivo; instead, such dendritic cells preferentially induce the expression of the TReg cell-specific transcription factor FOXP3, the surface marker CD25 and the anti-inflammatory cytokine IL-10 in naive T cells98,107,117 (Fig. 4). Such peripherally induced TReg cells profoundly affect the control of H. pylori, as shown in chronically infected patients119,120,121,122,123 and by animal experiments in which TReg cells are systemically depleted in infected hosts52,107. TReg cells accumulate in H. pylori-infected human gastric mucosa119,121, especially in children123 and in asymptomatic carriers122, and effectively suppress H. pylori-specific memory T cell responses120.
Experimental depletion of TReg cells facilitates the clearance of H. pylori in infected animals52 and enhances vaccine-induced protective immunity in vaccinated mice107. The TReg-facilitated persistence of H. pylori requires T cell-specific expression of IL-10; in fact, Il10−/− mice and a strain lacking IL-10 expression in the CD4+ T cell compartment are capable of spontaneously controlling experimental infections52,78,124. The efficient control or even clearance of H. pylori in animals invariably comes at the price of enhanced gastric immunopathology (gastritis and epithelial changes such as atrophy and intestinal metaplasia). Interestingly, an analogous observation has been reported for human carriers, which either accumulate large numbers of IL-10-producing, H. pylori-specific TReg cells and are colonized heavily (asymptomatic carriers), or develop gastric ulcers because their TReg cell response is inadequate122. The induction of H. pylori-specific tolerance to dendritic cells, which seems to be a prerequisite for the skewing of T cell responses (at least in experimental models98,117), requires the activity of both VacA and GGT116 (Fig. 4). Although the exact mechanism of VacA- and GGT-specific dendritic cell tolerance remains unclear, the newly assigned function of both factors in TReg cell induction and persistence is consistent with previous reports showing that gene deletion mutants lacking VacA or GGT have colonization defects relative to their parental VacA- or GGT-proficient wild-type isolates125,126.
Systemic consequences of immunosuppression
The active inhibition and manipulation of adaptive T cell-driven immune responses by H. pylori has various consequences for the host. The persistence mechanisms of H. pylori are dominant enough to override the protective effects conferred by H. pylori-specific vaccination; a challenge infection can only be cleared (or at least strongly reduced) by vaccinated mice if TReg cells or dendritic cells are depleted107. These observations partly explain the difficulties and obstacles faced in H. pylori vaccine development (Box 2). An interesting side effect of H. pylori-specific immunomodulation and manipulation is evident in Western societies from which H. pylori is gradually disappearing owing to reduced transmission rates, the frequent use of antibiotics in childhood and generally improved sanitation conditions127. In these populations, the incidence of allergic asthma, other allergic disease manifestations and chronic inflammatory diseases is steadily increasing, and an inverse association with H. pylori colonization has been documented for allergic asthma128,129,130,131,132 and inflammatory bowel diseases84 (Box 3). Although the exact mechanisms underlying this inverse association remain to be elucidated, the idea that H. pylori-induced immune regulation and manipulation are causally linked to protection from such immune disorders is compelling (Box 3). The fact that TReg cells that have been isolated from H. pylori-infected mice are sufficient to protect naive recipients against allergen-induced asthma in adoptive transfer models argues in favour of TReg-mediated cross-protection against allergen-specific immune responses98,133. Further work in this area is urgently needed to reveal the intricate interactions of this extraordinarily well-adapted persistent pathogen with the host adaptive immune system.
Conclusions and future perspectives
The work summarized in this Review outlines how H. pylori uses a combination of virulence factors and immune subversion and manipulation mechanisms to colonize and persist in the challenging environment of the gastric mucosa. Recent experimental work has elucidated exciting details on the structure and function of the T4SS, the pleiotropic effects of CagA delivery, the CagA-independent effects of the secretion system and newly discovered functions of the extracellular effector CagL. The role of cell shape and chemotaxis in persistent colonization is now well documented with respect to the genes involved. Progress in other areas, particularly H. pylori-specific vaccine development, has suffered from setbacks in Phase I clinical trials and from a lack of continuous industry support. The necessity of overriding the persistence strategies of the bacterium has been identified as a major challenge in H. pylori-specific vaccine development. Interest in the field has shifted towards gaining a better understanding of the benefits (suggested from epidemiological studies) that the infection may bestow on the large majority of asymptomatic carriers, and experimental evidence has been forthcoming to support such claims. In particular, it is now becoming increasingly clear that the virulence factors used by H. pylori and the mechanisms that are exploited to override T cell-driven immunity and to ensure persistent infection have systemic immunomodulatory effects that probably explain the benefits of the infection to asymptomatic carriers. The molecular mechanisms that allow H. pylori to suppress T cell activation through production of VacA and GGT, and to skew T cell responses towards regulatory T cells, are increasingly well understood.
Other aspects of the H. pylori–host interaction have received surprisingly little, if any, attention. These include the specifics of inflammasome activation by H. pylori and of innate immune activation by H. pylori in general, the molecular basis of host specificity, and the relative (or perhaps additive) contributions of its direct and indirect (inflammation-mediated) carcinogenic properties to gastric cancer development. Another important aspect of H. pylori biology that has been mostly ignored relates to its transmission. Although several independent, mostly older, studies indicate that mothers serve as the predominant source of their children's H. pylori infection, the transmission route remains unclear. Furthermore, little is currently known about the vast differences in the risk of gastric cancer development among human populations (often closely related and physically close), which is likely to be influenced by human genetic predisposition, population ecology and behaviour. In summary, many of the peculiarities that set H. pylori apart from other Gram-negative enteropathogens remain underexplored and deserve further work.
References
Wroblewski, L. E., Peek, R. M. Jr & Wilson, K. T. Helicobacter pylori and gastric cancer: factors that modulate disease risk. Clin. Microbiol. Rev. 23, 713–739 (2010).
Bik, E. M. et al. Molecular analysis of the bacterial microbiota in the human stomach. Proc. Natl Acad. Sci. USA 103, 732–737 (2006).
Palframan, S. L., Kwok, T. & Gabriel, K. Vacuolating cytotoxin A (VacA), a key toxin for Helicobacter pylori pathogenesis. Front. Cell. Infect. Microbiol. 2, 92 (2012).
Schreiber, S. et al. Rapid loss of motility of Helicobacter pylori in the gastric lumen in vivo. Infect. Immun. 73, 1584–1589 (2005).
Vaishnava, S. et al. The antibacterial lectin RegIIIgamma promotes the spatial segregation of microbiota and host in the intestine. Science 334, 255–258 (2011).
Montecucco, C. & Rappuoli, R. Living dangerously: how Helicobacter pylori survives in the human stomach. Nature Rev. Mol. Cell Biol. 2, 457–466 (2001).
Celli, J. P. et al. Rheology of gastric mucin exhibits a pH-dependent sol-gel transition. Biomacromolecules 8, 1580–1586 (2007).
Celli, J. P. et al. Helicobacter pylori moves through mucus by reducing mucin viscoelasticity. Proc. Natl Acad. Sci. USA 106, 14321–14326 (2009). Study showing that H. pylori is immobilized by gastric mucin gel at low pH but in the presence of urea induces a pH-dependent gel-to-solution transition that allows the bacterium to swim freely.
Howitt, M. R. et al. ChePep controls Helicobacter pylori infection of the gastric glands and chemotaxis in the Epsilonproteobacteria. mBio 26 Jul 2011 (doi:10.1128/mBio.00098-1).
Rolig, A. S., Carter, J. E. & Ottemann, K. M. Bacterial chemotaxis modulates host cell apoptosis to establish a T-helper cell, type 17 (Th17)-dominant immune response in Helicobacter pylori infection. Proc. Natl Acad. Sci. USA 108, 19749–19754 (2011). Study demonstrating that chemotaxis promotes interactions between the bacteria and epithelium that drive pro-inflammatory T H 17 responses.
Rolig, A. S., Shanks, J., Carter, J. E. & Ottemann, K. M. Helicobacter pylori requires TlpD-driven chemotaxis to proliferate in the antrum. Infect. Immun. 80, 3713–3720 (2012).
Terry, K., Williams, S. M., Connolly, L. & Ottemann, K. M. Chemotaxis plays multiple roles during Helicobacter pylori animal infection. Infect. Immun. 73, 803–811 (2005).
Bonis, M., Ecobichon, C., Guadagnini, S., Prevost, M. C. & Boneca, I. G. A. M23B family metallopeptidase of Helicobacter pylori required for cell shape, pole formation and virulence. Mol. Microbiol. 78, 809–819 (2010).
Sycuro, L. K. et al. Peptidoglycan crosslinking relaxation promotes Helicobacter pylori's helical shape and stomach colonization. Cell 141, 822–833 (2010). References 13 and 14 first identified cell wall enzymes that reduce crosslinking in the cell wall and that promote helical cell shape, which in turn promotes efficient stomach colonization.
Sycuro, L. K. et al. Multiple peptidoglycan modification networks modulate Helicobacter pylori's cell shape, motility, and colonization potential. PLoS Pathog. 8, e1002603 (2012).
Williams, S. M. et al. Helicobacter pylori chemotaxis modulates inflammation and bacterium-gastric epithelium interactions in infected mice. Infect. Immun. 75, 3747–3757 (2007).
Sayi, A. et al. The CD4+ T cell-mediated IFN-gamma response to Helicobacter infection is essential for clearance and determines gastric cancer risk. J. Immunol. 182, 7085–7101 (2009). This paper revealed that T cell responses to H. pylori promote clearance on the one hand and immunopathology on the other hand, which complicates vaccine development.
Gobert, A. P. et al. Helicobacter pylori arginase inhibits nitric oxide production by eukaryotic cells: a strategy for bacterial survival. Proc. Natl Acad. Sci. USA 98, 13844–13849 (2001).
Wang, G., Alamuri, P. & Maier, R. J. The diverse antioxidant systems of Helicobacter pylori. Mol. Microbiol. 61, 847–860 (2006).
Dorer, M. S., Sessler, T. H. & Salama, N. R. Recombination and DNA repair in Helicobacter pylori. Annu. Rev. Microbiol. 65, 329–348 (2011).
Chaturvedi, R. et al. Spermine oxidase mediates the gastric cancer risk associated with Helicobacter pylori CagA. Gastroenterology 141, 1696–1708 (2011).
Touati, E. et al. Chronic Helicobacter pylori infections induce gastric mutations in mice. Gastroenterology 124, 1408–1419 (2003).
Dorer, M. S., Fero, J. & Salama, N. R. DNA damage triggers genetic exchange in Helicobacter pylori. PLoS Pathog. 6, e1001026 (2010).
Orillard, E., Radicella, J. P. & Marsin, S. Biochemical and cellular characterization of Helicobacter pylori RecA, a protein with high-level constitutive expression. J. Bacteriol. 193, 6490–6497 (2011).
Dorer, M. S., Cohen, I. E., Sessler, T. H., Fero, J. & Salama, N. R. Natural competence promotes Helicobacter pylori chronic infection. Infect. Immun. 81, 209–215 (2012).
Aras, R. A., Kang, J., Tschumi, A. I., Harasaki, Y. & Blaser, M. J. Extensive repetitive DNA facilitates prokaryotic genome plasticity. Proc. Natl Acad. Sci. USA 100, 13579–13584 (2003).
Aras, R. A. et al. Plasticity of repetitive DNA sequences within a bacterial (Type IV) secretion system component. J. Exp. Med. 198, 1349–1360 (2003).
Barrozo, R. M. et al. Functional plasticity in the Type IV secretion system of Helicobacter pylori. PLoS Pathog. 9, e1003189 (2013).
Alm, R. A. et al. Comparative genomics of Helicobacter pylori: analysis of the outer membrane protein families. Infect. Immun. 68, 4155–4168 (2000).
Colbeck, J. C., Hansen, L. M., Fong, J. M. & Solnick, J. V. Genotypic profile of the outer membrane proteins BabA and BabB in clinical isolates of Helicobacter pylori. Infect. Immun. 74, 4375–4378 (2006).
Hennig, E. E., Allen, J. M. & Cover, T. L. Multiple chromosomal loci for the babA gene in Helicobacter pylori. Infect. Immun. 74, 3046–3051 (2006).
Solnick, J. V., Hansen, L. M., Salama, N. R., Boonjakuakul, J. K. & Syvanen, M. Modification of Helicobacter pylori outer membrane protein expression during experimental infection of rhesus macaques. Proc. Natl Acad. Sci. USA 101, 2106–2111 (2004). This was the first demonstration of gene conversion as a mechanism for phase variation of adhesin expression during experimental infection.
Ilver, D. et al. Helicobacter pylori adhesin binding fucosylated histo-blood group antigens revealed by retagging. Science 279, 373–377 (1998).
Kawai, M. et al. Evolution in an oncogenic bacterial species with extreme genome plasticity: Helicobacter pylori East Asian genomes. BMC Microbiol. 11, 104 (2011).
Mahdavi, J. et al. Helicobacter pylori SabA adhesin in persistent infection and chronic inflammation. Science 297, 573–578 (2002).
Talarico, S., Whitefield, S. E., Fero, J., Haas, R. & Salama, N. R. Regulation of Helicobacter pylori adherence by gene conversion. Mol. Microbiol. 84, 1050–1061 (2012).
Styer, C. M. et al. Expression of the BabA adhesin during experimental infection with Helicobacter pylori. Infect. Immun. 78, 1593–1600 (2010).
Goodwin, A. C. et al. Expression of the Helicobacter pylori adhesin SabA is controlled via phase variation and the ArsRS signal transduction system. Microbiology 154, 2231–2240 (2008).
Salaun, L., Ayraud, S. & Saunders, N. J. Phase variation mediated niche adaptation during prolonged experimental murine infection with Helicobacter pylori. Microbiology 151, 917–923 (2005).
Kao, C. Y., Sheu, S. M., Sheu, B. S. & Wu, J. J. Length of thymidine homopolymeric repeats modulates promoter activity of sabA in Helicobacter pylori. Helicobacter 17, 203–209 (2012).
Covacci, A. et al. Molecular characterization of the 128-kDa immunodominant antigen of Helicobacter pylori associated with cytotoxicity and duodenal ulcer. Proc. Natl Acad. Sci. USA 90, 5791–5795 (1993).
Tummuru, M. K., Cover, T. L. & Blaser, M. J. Cloning and expression of a high-molecular-mass major antigen of Helicobacter pylori: evidence of linkage to cytotoxin production. Infect. Immun. 61, 1799–1809 (1993).
Murata-Kamiya, N. Pathophysiological functions of the CagA oncoprotein during infection by Helicobacter pylori. Microbes Infect. 13, 799–807 (2011).
Ohnishi, N. et al. Transgenic expression of Helicobacter pylori CagA induces gastrointestinal and hematopoietic neoplasms in mouse. Proc. Natl Acad. Sci. USA 105, 1003–1008 (2008). A study using transgenic expression to show that CagA can behave as an oncogene.
Yamazaki, S. et al. The CagA protein of Helicobacter pylori is translocated into epithelial cells and binds to SHP-2 in human gastric mucosa. J. Infect. Dis. 187, 334–337 (2003).
Tsugawa, H. et al. Reactive oxygen species-induced autophagic egradation of Helicobacter pylori CagA is specifically suppressed in cancer stem-like cells. Cell Host Microbe 12, 764–777 (2012). This study defines a molecular interaction by which certain alleles of VacA attenuate CagA activity in cells through autophagy-dependent degradation. These results provide a possible mechanism for the observed association between carriage of CagA and VacA s1m1 alleles. Additionally, the identification of stem-like cells that are resistant to VacA s1m1 autophagy induction indicate a possible CagA-dependent cancer precursor.
Ishimoto, T. et al. CD44 variant regulates redox status in cancer cells by stabilizing the xCT subunit of system xc(-) and thereby promotes tumor growth. Cancer Cell 19, 387–400 (2011).
Oh, J. D., Karam, S. M. & Gordon, J. I. Intracellular Helicobacter pylori in gastric epithelial progenitors. Proc. Natl Acad. Sci. USA 102, 5186–5191 (2005).
Hayashi, T., Morohashi, H. & Hatakeyama, M. Bacterial EPIYA effectors - Where do they come from? What are they? Where are they going? Cell. Microbiol. 15, 377–385 (2012).
Mueller, D. et al. c-Src and c-Abl kinases control hierarchic phosphorylation and function of the CagA effector protein in Western and East Asian Helicobacter pylori strains. J. Clin. Invest. 122, 1553–1566 (2012). Mutational analysis demonstrating that SRC and ABL family kinases phosphorylate CagA sequentially and in a tightly controlled manner.
Israel, D. A. et al. Helicobacter pylori strain-specific differences in genetic content, identified by microarray, influence host inflammatory responses. J. Clin. Invest. 107, 611–620 (2001).
Arnold, I. C. et al. Tolerance rather than immunity protects from Helicobacter pylori-induced gastric preneoplasia. Gastroenterology 140, 199–209 (2011).
Philpott, D. J. et al. Reduced activation of inflammatory responses in host cells by mouse-adapted Helicobacter pylori isolates. Cell. Microbiol. 4, 285–296 (2002).
Tan, S., Noto, J. M., Romero-Gallo, J., Peek, R. M. Jr & Amieva, M. R. Helicobacter pylori perturbs iron trafficking in the epithelium to grow on the cell surface. PLoS Pathog. 7, e1002050 (2011).
Terradot, L. & Waksman, G. Architecture of the Helicobacter pylori Cag-type IV secretion system. FEBS J. 278, 1213–1222 (2011).
Christie, P. J., Atmakuri, K., Krishnamoorthy, V., Jakubowski, S. & Cascales, E. Biogenesis, architecture, and function of bacterial type IV secretion systems. Annu. Rev. Microbiol. 59, 451–485 (2005).
Chandran, V. et al. Structure of the outer membrane complex of a type IV secretion system. Nature 462, 1011–1015 (2009).
Fischer, W. et al. Systematic mutagenesis of the Helicobacter pylori cag pathogenicity island: essential genes for CagA translocation in host cells and induction of interleukin-8. Mol. Microbiol. 42, 1337–1348 (2001).
Pham, K. T. et al. CagI is an essential component of the Helicobacter pylori Cag type IV secretion system and forms a complex with CagL. PLoS ONE 7, e35341 (2012).
Rohde, M., Puls, J., Buhrdorf, R., Fischer, W. & Haas, R. A novel sheathed surface organelle of the Helicobacter pylori cag type IV secretion system. Mol. Microbiol. 49, 219–234 (2003).
Tanaka, J., Suzuki, T., Mimuro, H. & Sasakawa, C. Structural definition on the surface of Helicobacter pylori type IV secretion apparatus. Cell. Microbiol. 5, 395–404 (2003).
Kwok, T. et al. Helicobacter exploits integrin for type IV secretion and kinase activation. Nature 449, 862–866 (2007). This was the first demonstration that CagL can interact with integrins and has multiple roles in CagA secretion and Cag T4SS-dependent pathological effects on host cells.
Conradi, J. et al. An RGD helper sequence in CagL of Helicobacter pylori assists in interactions with integrins and injection of CagA. Front. Cell. Infect. Microbiol. 2, 70 (2012).
Shaffer, C. L. et al. Helicobacter pylori exploits a unique repertoire of type IV secretion system components for pilus assembly at the bacteria-host cell interface. PLoS Pathog. 7, e1002237 (2011). A study describing robust methods to visualize Cag T4SS pili, revealing that CagA secretion and Cag pilus formation can be uncoupled.
Jimenez-Soto, L. F. et al. Helicobacter pylori type IV secretion apparatus exploits beta1 integrin in a novel RGD-independent manner. PLoS Pathog. 5, e1000684 (2009).
Kaplan-Turkoz, B. et al. Structural insights into Helicobacter pylori oncoprotein CagA interaction with beta1 integrin. Proc. Natl Acad. Sci. USA 109, 14640–14645 (2012).
Gorrell, R. J. et al. A novel NOD1- and CagA-independent pathway of interleukin-8 induction mediated by the Helicobacter pylori type IV secretion system. Cell Microbiol. 26 Oct 2012 (doi:10.1111/cmi.12055).
Saha, A., Backert, S., Hammond, C. E., Gooz, M. & Smolka, A. J. Helicobacter pylori CagL activates ADAM17 to induce repression of the gastric H, K-ATPase alpha subunit. Gastroenterology 139, 239–248 (2010).
Tegtmeyer, N. et al. A small fibronectin-mimicking protein from bacteria induces cell spreading and focal adhesion formation. J. Biol. Chem. 285, 23515–23526 (2010).
Wiedemann, T. et al. Helicobacter pylori CagL dependent induction of gastrin expression via a novel alphavbeta5-integrin-integrin linked kinase signalling complex. Gut 61, 986–996 (2012).
Moran, A. P., Lindner, B. & Walsh, E. J. Structural characterization of the lipid A component of Helicobacter pylori rough- and smooth-form lipopolysaccharides. J. Bacteriol. 179, 6453–6463 (1997).
Cullen, T. W. et al. Helicobacter pylori versus the host: remodeling of the bacterial outer membrane is required for survival in the gastric mucosa. PLoS Pathog. 7, e1002454 (2012). This paper provides the first description of the H. pylori phosphatases that are responsible for the modification of lipid A that allows escape from TLR4 recognition and mouse colonization.
Ishihara, S. et al. Essential role of MD-2 in TLR4-dependent signaling during Helicobacter pylori-associated gastritis. J. Immunol. 173, 1406–1416 (2004).
Kawahara, T. et al. Type I Helicobacter pylori lipopolysaccharide stimulates toll-like receptor 4 and activates mitogen oxidase 1 in gastric pit cells. Infect. Immun. 69, 4382–4389 (2001).
Yokota, S. et al. Highly-purified Helicobacter pylori LPS preparations induce weak inflammatory reactions and utilize Toll-like receptor 2 complex but not Toll-like receptor 4 complex. FEMS Immunol. Med. Microbiol. 51, 140–148 (2007).
Smith, S. M. et al. Tribbles 3: a novel regulator of TLR2-mediated signaling in response to Helicobacter pylori lipopolysaccharide. J. Immunol. 186, 2462–2471 (2011).
Rad, R. et al. Extracellular and intracellular pattern recognition receptors cooperate in the recognition of Helicobacter pylori. Gastroenterology 136, 2247–2257 (2009). This article provides a comprehensive analysis of innate immune recognition of H. pylori using dendritic cells from gene-targeted mice lacking various combinations of PRRs.
Sayi, A. et al. TLR-2-activated B cells suppress Helicobacter-induced preneoplastic gastric immunopathology by inducing T regulatory-1 cells. J. Immunol. 186, 878–890 (2011).
Gewirtz, A. T. et al. Helicobacter pylori flagellin evades toll-like receptor 5-mediated innate immunity. J. Infect. Dis. 189, 1914–1920 (2004).
Andersen-Nissen, E. et al. Evasion of Toll-like receptor 5 by flagellated bacteria. Proc. Natl Acad. Sci. USA 102, 9247–9252 (2005).
Otani, K. et al. Toll-like receptor 9 signaling has anti-inflammatory effects on the early phase of Helicobacter pylori-induced gastritis. Biochem. Biophys. Res. Commun. 426, 342–349 (2012).
Owyang, S. Y., Luther, J., Owyang, C. C., Zhang, M. & Kao, J. Y. Helicobacter pylori DNA's anti-inflammatory effect on experimental colitis. Gut Microbes 3, 168–171 (2012).
Luther, J. et al. Helicobacter pylori DNA decreases pro-inflammatory cytokine production by dendritic cells and attenuates dextran sodium sulphate-induced colitis. Gut 60, 1479–1486 (2011).
Luther, J., Dave, M., Higgins, P. D. & Kao, J. Y. Association between Helicobacter pylori infection and inflammatory bowel disease: a meta-analysis and systematic review of the literature. Inflamm Bowel Dis. 16, 1077–1084 (2010).
Gringhuis, S. I., den Dunnen, J., Litjens, M., van der Vlist, M. & Geijtenbeek, T. B. Carbohydrate-specific signaling through the DC-SIGN signalosome tailors immunity to Mycobacterium tuberculosis, HIV-1 and Helicobacter pylori. Nature Immunol. 10, 1081–1088 (2009).
Gringhuis, S. I. et al. C-type lectin DC-SIGN modulates Toll-like receptor signaling via Raf-1 kinase-dependent acetylation of transcription factor NF-kappaB. Immunity 26, 605–616 (2007).
Strowig, T., Henao-Mejia, J., Elinav, E. & Flavell, R. Inflammasomes in health and disease. Nature 481, 278–286 (2012).
Kim, Y. G. et al. The cytosolic sensors Nod1 and Nod2 are critical for bacterial recognition and host defense after exposure to Toll-like receptor ligands. Immunity 28, 246–257 (2008).
Broz, P. & Monack, D. M. Molecular mechanisms of inflammasome activation during microbial infections. Immunol. Rev. 243, 174–190 (2011).
Viala, J. et al. Nod1 responds to peptidoglycan delivered by the Helicobacter pylori cag pathogenicity island. Nature Immunol. 5, 1166–1174 (2004).
Kaparakis, M. et al. Bacterial membrane vesicles deliver peptidoglycan to NOD1 in epithelial cells. Cell. Microbiol. 12, 372–385 (2009).
Hutton, M. L. et al. Helicobacter pylori exploits cholesterol-rich microdomains for induction of NF-kappaB-dependent responses and peptidoglycan delivery in epithelial cells. Infect. Immun. 78, 4523–4531 (2010).
Allison, C. C., Kufer, T. A., Kremmer, E., Kaparakis, M. & Ferrero, R. L. Helicobacter pylori induces MAPK phosphorylation and AP-1 activation via a NOD1-dependent mechanism. J. Immunol. 183, 8099–8109 (2009).
Grubman, A. et al. The innate immune molecule, NOD1, regulates direct killing of Helicobacter pylori by antimicrobial peptides. Cell. Microbiol. 12, 626–639 (2009).
Watanabe, T. et al. NOD1 contributes to mouse host defense against Helicobacter pylori via induction of type I IFN and activation of the ISGF3 signaling pathway. J. Clin. Invest. 120, 1645–1662 (2010). This article provides a description of a new signalling pathway linking NOD1 activation by H. pylori to type I IFN production and infection control.
Hitzler, I. et al. Caspase-1 has both proinflammatory and regulatory properties in Helicobacter infections, which are differentially mediated by its substrates IL-1beta and IL-18. J. Immunol. 188, 3594–3602 (2012).
Tomita, T. et al. Expression of Interleukin-18, a Th1 cytokine, in human gastric mucosa is increased in Helicobacter pylori infection. J. Infect. Dis. 183, 620–627 (2001).
Oertli, M. et al. DC-derived IL-18 drives Treg differentiation, murine Helicobacter pylori-specific immune tolerance, and asthma protection. J. Clin. Invest. 122, 1082–1096 (2012).
Tu, S. et al. Overexpression of interleukin-1beta induces gastric inflammation and cancer and mobilizes myeloid-derived suppressor cells in mice. Cancer Cell 14, 408–419 (2008).
El-Omar, E. M. et al. Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature 404, 398–402 (2000).
Benoit, B. N. et al. Role of ASC in the mouse model of Helicobacter pylori infection. J. Histochem. Cytochem. 57, 327–338 (2009).
Akhiani, A. A. et al. Protection against Helicobacter pylori infection following immunization is IL-12-dependent and mediated by Th1 cells. J. Immunol. 169, 6977–6984 (2002).
Akhiani, A. A., Schon, K., Franzen, L. E., Pappo, J. & Lycke, N. Helicobacter pylori-specific antibodies impair the development of gastritis, facilitate bacterial colonization, and counteract resistance against infection. J. Immunol. 172, 5024–5033 (2004).
Ermak, T. H. et al. Immunization of mice with urease vaccine affords protection against Helicobacter pylori infection in the absence of antibodies and is mediated by MHC class II-restricted responses. J. Exp. Med. 188, 2277–2288 (1998).
Velin, D., Bachmann, D., Bouzourene, H. & Michetti, P. Mast cells are critical mediators of vaccine-induced Helicobacter clearance in the mouse model. Gastroenterology 129, 142–155 (2005).
Velin, D. et al. Interleukin-17 is a critical mediator of vaccine-induced reduction of Helicobacter infection in the mouse model. Gastroenterology 136, 2237–2246 (2009).
Hitzler, I., Oertli, M., Becher, B., Agger, E. M. & Müller, A. Dendritic cells prevent. rather than promote immunity conferred by a Helicobacter vaccine using a mycobacterial adjuvant. Gastroenterology 141, 186–196 (2011).
Shi, Y. et al. Helicobacter pylori-induced Th17 responses modulate Th1 cell responses, benefit bacterial growth, and contribute to pathology in mice. J. Immunol. 184, 5121–5129 (2010).
Stoicov, C. et al. T-bet knockout prevents Helicobacter felis-induced gastric cancer. J. Immunol. 183, 642–649 (2009).
Gebert, B., Fischer, W., Weiss, E., Hoffmann, R. & Haas, R. Helicobacter pylori vacuolating cytotoxin inhibits T lymphocyte activation. Science 301, 1099–1102 (2003).
Sundrud, M. S., Torres, V. J., Unutmaz, D. & Cover, T. L. Inhibition of primary human T cell proliferation by Helicobacter pylori vacuolating toxin (VacA) is independent of VacA effects on IL-2 secretion. Proc. Natl Acad. Sci. USA 101, 7727–7732 (2004).
Sewald, X. et al. Integrin subunit CD18 Is the T-lymphocyte receptor for the Helicobacter pylori vacuolating cytotoxin. Cell Host Microbe 3, 20–29 (2008).
Sewald, X., Jimenez-Soto, L. & Haas, R. PKC-dependent endocytosis of the Helicobacter pylori vacuolating cytotoxin in primary T lymphocytes. Cell. Microbiol. 13, 482–496 (2010).
Gerhard, M. et al. A secreted low-molecular-weight protein from Helicobacter pylori induces cell-cycle arrest of T cells. Gastroenterology 128, 1327–1339 (2005).
Schmees, C. et al. Inhibition of T-cell proliferation by Helicobacter pylori gamma-glutamyl transpeptidase. Gastroenterology 132, 1820–1833 (2007).
Oertli, M. et al. Helicobacter pylori gamma-glutamyl transpeptidase and vacuolating cytotoxin promote gastric persistence and immune tolerance. Proc. Natl Acad. Sci. USA 110, 3047–3052 (2013).
Kao, J. Y. et al. Helicobacter pylori immune escape is mediated by dendritic cell-induced Treg skewing and Th17 suppression in mice. Gastroenterology 138, 1046–1054 (2010).
Kim, J. M. et al. Stimulation of dendritic cells with Helicobacter pylori vacuolating cytotoxin negatively regulates their maturation via the restoration of E2F1. Clin. Exp. Immunol. 166, 34–45 (2011).
Lundgren, A. et al. Mucosal FOXP3-expressing CD4+ CD25high regulatory T cells in Helicobacter pylori-infected patients. Infect. Immun. 73, 523–531 (2005).
Lundgren, A., Suri-Payer, E., Enarsson, K., Svennerholm, A. M. & Lundin, B. S. Helicobacter pylori-specific CD4+ CD25high regulatory T cells suppress memory T-cell responses to H. pylori in infected individuals. Infect. Immun. 71, 1755–1762 (2003).
Lundgren, A., Trollmo, C., Edebo, A., Svennerholm, A. M. & Lundin, B. S. Helicobacter pylori-specific CD4+ T cells home to and accumulate in the human Helicobacter pylori-infected gastric mucosa. Infect. Immun. 73, 5612–5619 (2005).
Robinson, K. et al. Helicobacter pylori-induced peptic ulcer disease is associated with inadequate regulatory T cell responses. Gut 57, 1375–1385 (2008). This study demonstrates that asymptomatic carriers predominantly launch T Reg responses to H. pylori infection, whereas patients with peptic ulcer disease generate effector T cell responses.
Harris, P. R. et al. Helicobacter pylori gastritis in children is associated with a regulatory T-cell response. Gastroenterology 134, 491–499 (2008).
Ismail, H. F., Fick, P., Zhang, J., Lynch, R. G. & Berg, D. J. Depletion of neutrophils in IL-10(−/−) mice delays clearance of gastric Helicobacter infection and decreases the Th1 immune response to Helicobacter. J. Immunol. 170, 3782–3789 (2003).
Salama, N. R., Otto, G., Tompkins, L. & Falkow, S. Vacuolating cytotoxin of Helicobacter pylori plays a role during colonization in a mouse model of infection. Infect. Immun. 69, 730–736 (2001).
Chevalier, C., Thiberge, J. M., Ferrero, R. L. & Labigne, A. Essential role of Helicobacter pylori gamma-glutamyltranspeptidase for the colonization of the gastric mucosa of mice. Mol. Microbiol. 31, 1359–1372 (1999).
Blaser, M. J. & Falkow, S. What are the consequences of the disappearing human microbiota? Nature Rev. Microbiol. 7, 887–894 (2009).
Amberbir, A. et al. Effects of Helicobacter pylori, geohelminth infection and selected commensal bacteria on the risk of allergic disease and sensitization in 3-year-old Ethiopian children. Clin. Exp. Allergy 41, 1422–1430 (2011).
Blaser, M. J., Chen, Y. & Reibman, J. Does Helicobacter pylori protect against asthma and allergy? Gut 57, 561–567 (2008).
Chen, Y. & Blaser, M. J. Inverse associations of Helicobacter pylori with asthma and allergy. Arch. Intern. Med. 167, 821–827 (2007).
Chen, Y. & Blaser, M. J. Helicobacter pylori colonization is inversely associated with childhood asthma. J. Infect. Dis. 198, 553–560 (2008).
Reibman, J. et al. Asthma is inversely associated with Helicobacter pylori status in an urban population. PLoS ONE 3, e4060 (2008).
Arnold, I. C. et al. Helicobacter pylori infection prevents allergic asthma in mouse models through the induction of regulatory T cells. J. Clin. Invest. 121, 3088–3093 (2011). This paper provides the first experimental evidence of a protective effect of H. pylori infection in allergic asthma.
Hayashi, T. et al. Tertiary structure-function analysis reveals the pathogenic signaling potentiation mechanism of Helicobacter pylori oncogenic effector CagA. Cell Host Microbe 12, 20–33 (2012). This study uses a combination of NMR, X-ray crystallography, modelling and mutational analysis to reveal the molecular mechanisms by which CagA interacts with multiple cellular targets.
Murata-Kamiya, N., Kikuchi, K., Hayashi, T., Higashi, H. & Hatakeyama, M. Helicobacter pylori exploits host membrane phosphatidylserine for delivery, localization, and pathophysiological action of the CagA oncoprotein. Cell Host Microbe 7, 399–411 (2010).
Olbermann, P. et al. A global overview of the genetic and functional diversity in the Helicobacter pylori cag pathogenicity island. PLoS Genet. 6, e1001069 (2010).
de Sablet, T. et al. Phylogeographic origin of Helicobacter pylori is a determinant of gastric cancer risk. Gut 60, 1189–1195 (2011).
Yeh, Y. C. et al. H. pylori cagL amino acid sequence polymorphism Y58E59 induces a corpus shift of gastric integrin alpha5beta1 related with gastric carcinogenesis. Mol. Carcinog. 50, 751–759 (2011).
Rizzato, C. et al. Variations in Helicobacter pylori cytotoxin-associated genes and their influence in progression to gastric cancer: implications for prevention. PLoS ONE 7, e29605 (2012).
Rupnow, M. F., Chang, A. H., Shachter, R. D., Owens, D. K. & Parsonnet, J. Cost-effectiveness of a potential prophylactic Helicobacter pylori vaccine in the United States. J. Infect. Dis. 200, 1311–1317 (2009).
Muller, A. & Solnick, J. V. Inflammation, immunity, and vaccine development for Helicobacter pylori. Helicobacter 16 (Suppl. 1), 26–32 (2011).
Czinn, S. J. & Blanchard, T. Vaccinating against Helicobacter pylori infection. Nature Rev. Gastroenterol. Hepatol 8, 133–140 (2011).
Aebischer, T. et al. Correlation of T cell response and bacterial clearance in human volunteers challenged with Helicobacter pylori revealed by randomised controlled vaccination with Ty21a-based Salmonella vaccines. Gut 57, 1065–1072 (2008). This article describes the first human vaccine trial in which volunteers were challenged with live H. pylori ; it also provides the first evidence that T cells are required for H. pylori infection control in humans.
Malfertheiner, P. et al. Safety and immunogenicity of an intramuscular Helicobacter pylori vaccine in noninfected volunteers: a phase I study. Gastroenterology 135, 787–795 (2008).
Linz, B. et al. An African origin for the intimate association between humans and Helicobacter pylori. Nature 445, 915–918 (2007).
Howson, C. P., Hiyama, T. & Wynder, E. L. The decline in gastric cancer: epidemiology of an unplanned triumph. Epidemiol. Rev. 8, 1–27 (1986).
Herbarth, O. et al. Helicobacter pylori colonisation and eczema. J. Epidemiol. Commun. Health 61, 638–640 (2007).
Higgins, P. D. et al. Prior Helicobacter pylori infection ameliorates Salmonella typhimurium-induced colitis: Mucosal crosstalk between stomach and distal intestine. Inflamm. Bowel Dis. 17, 1398–1408 (2010).
Acknowledgements
Work in the laboratories of N.R.S. and A.M. is supported by grants AI054423 and AI094839 from the US National Institutes of Health to N.R.S. and grants from the Swiss and Zurich Cantonal Cancer Leagues, the Gebert-Rüf Foundation and the Swiss National Science Foundation to A.M. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of these funding agencies.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
FURTHER INFORMATION
Glossary
- Mucosa-associated lymphoid tissue lymphoma
-
A cancer originating from marginal zone B cells of mucosa-associated lymphoid tissue. Helicobacter pylori infection is tightly associated with these lymphomas, which can be treated with H. pylori eradication therapy to eliminate antigenic drive.
- Gastric adenocarcinoma
-
A malignant epithelial tumour that originates from the glandular epithelium of the stomach.
- SOS response
-
A coordinated transcriptional response to DNA damage that is extensively characterized in Escherichia coli and is initiated by activation of RecA through binding to damaged DNA, resulting in the inhibition of cell cycle progression and increased expression of DNA repair proteins and mutagenic DNA polymerases.
- Natural competence
-
The ability to take up extracellular DNA and recombine it into the bacterial chromosome.
- Type IV secretion system
-
(T4SS). A Gram-negative bacterial contact-dependent specialized secretion system that is evolutionarily related to the Agrobacterium tumefaciens transforming plasmid pilus. These multisubunit molecular machines deliver proteins and/or protein–DNA complexes from the bacterial cytoplasm, across the bacterial cell wall (inner membrane, periplasm and outer membrane) and across a target eukaryotic cell plasma membrane to the target cell cytosol.
- Gene conversion
-
An intragenomic recombination event where gene sequences at one position in the genome are replaced with homologous sequences encoded at a different location.
- Slipped strand mispairing
-
A mutagenic process that can occur during DNA replication of dinucleotide or homopolymeric repeats due to mispairing of complementary bases.
- Cell polarity
-
Epithelial cells form connections between cells that restrict free diffusion both within the membrane and between cells, resulting in an apical surface orientated towards the lumen and a basolateral surface orientated towards the underlying submucosa.
- Pathogenicity island
-
(PAI). A genomic island that often encodes virulence determinants and that is typically acquired by horizontal transfer.
- Polarized cell culture model
-
A monolayer of cultured epithelial cells that form tight junctions. The cells are usually grown on filters that allow the apical and basolateral compartments to be accessed separately.
- Transcytosis
-
The movement of molecules across an epithelial cell, including uptake from the apical compartment and delivery to the basolateral compartment.
- Transmission electron microscopy
-
A microscopy technique that transmits a beam of electrons through an ultra-thin specimen and that is capable of imaging at much higher resolution than light microscopy.
- Field emission scanning electron microscopy
-
An electron microscopy technique in which an image is produced by scanning the sample with a focused beam of electrons using a field emission gun that generates a smaller diameter beam.
- Fibronectin
-
An extracellular matrix protein that binds integrins.
- Pathogen-associated molecular patterns
-
(PAMPs). These molecules have shared molecular motifs that are conserved among certain microorganisms and are detected by innate immune receptors; examples include lipopolysaccharide, lipoteichoic acid, flagellins, double-stranded RNA and hypomethylated CpG dinucleotides.
- Pattern recognition receptors
-
(PRRs). Surface-localized, endosomal or cytoplasmic receptors that are expressed by innate immune cells and recognize pathogen-associated or damage-associated molecular patterns; PRRs are classified according to their ligand specificity, function, localization and/or evolutionary relationships.
- Dendritic cells
-
Innate immune cells of characteristic morphology that serve as antigen-presenting cells; immature dendritic cells constantly sample their environment for invading microorganisms, which are phagocytosed and their antigens are processed and presented to T cells following migration to lymphoid organs.
- Type I interferons
-
(Type I IFNs). Synonymous with IFNα and IFNβ. Cytokines that are expressed by many leukocytes, large quantities of which are derived from plasmacytoid dendritic cells. They have an important role in antiviral defences through their activity on natural killer cells and macrophages.
- Sterilizing immunity
-
Protective immunity that results in complete clearance of the pathogen to below the detection limit, as opposed to a mere reduction in colonization levels.
- Adjuvants
-
Pharmacological or immunological agents that are added to vaccine formulations to improve their immunogenicity.
- Myeloid differentiation primary response gene 88
-
(MYD88). A cytoplasmic adaptor protein that couples ligand-activated Toll-like receptors (except TLR3) to downstream signalling pathways ultimately leading to nuclear factor-κB activation.
- Damage-associated molecular patterns
-
Also known as danger-associated molecular patterns. They are produced under inflammatory conditions of non-infectious origin or by damaged or stressed tissues. For example, proteins (such as heat shock proteins and S100 proteins), other macromolecules (extracellular or cytoplasmic DNA), ATP, adenosine and uric acid crystals.
- Inflammasomes
-
Large cytoplasmic multiprotein complexes that sense microbial infections or danger molecules and initiate auto-proteolytic cleavage of caspase 1, and the subsequent processing and release of pro-inflammatory cytokines, namely interleukin-1β and IL-18. Various types of inflammasome can be distinguished based on the NOD-like receptor involved in their activation.
- Outer-membrane vesicles
-
(OMVs). Also known as 'blebs'. Shed from the outer membrane of Gram-negative bacteria during normal growth, they have been reported to enter and transport virulence factors into host cells. OMVs contain numerous components of the bacterial cell wall, including peptidoglycan.
- Regulatory T cell
-
(TReg cell). A subpopulation of mostly CD4+CD25+FOXP3+ T cells that suppress immune responses by other cells, maintain self-tolerance and immune homeostasis, and prevent autoimmunity and excessive immunopathology. The lineage-defining transcription factor of TReg cells is FOXP3.
- Polarized effector T cell subsets
-
Following activation through their T cell receptor, T cells can differentiate into one of several T helper subtypes, including TH1, TH2 and TH17 cells, which differ in their lineage-defining transcription factors and cytokine expression profiles. The cytokine 'cocktail' provided by the antigen-presenting cell during T cell activation determines the TH subset polarization and differentiation.
- RAS signalling pathway
-
RAS is the prototypical member of the RAS superfamily of small GTPases. RAS-regulated signalling pathways control various cellular processes, including actin cytoskeletal rearrangements, proliferation, differentiation, cell adhesion, apoptosis and cell migration. RAS and RAS-related proteins are often deregulated in cancers.
- Naive T cells
-
T cells that have not yet come into contact with their cognate antigen.
- Methacholine
-
Muscarinic receptor agonist that is clinically used to diagnose bronchial hyperreactivity, a hallmark of asthma and of chronic obstructive pulmonary disease. The methacholine challenge test involves inhalation of aerosolized methacholine, which leads to bronchoconstriction.
Rights and permissions
About this article
Cite this article
Salama, N., Hartung, M. & Müller, A. Life in the human stomach: persistence strategies of the bacterial pathogen Helicobacter pylori. Nat Rev Microbiol 11, 385–399 (2013). https://doi.org/10.1038/nrmicro3016
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrmicro3016
This article is cited by
-
Recent Developments in Metallic Degradable Micromotors for Biomedical and Environmental Remediation Applications
Nano-Micro Letters (2024)
-
Anthocyanin-rich black carrot (Daucus carota ssp. sativus var. atrorubens Alef.) and red cabbage (Brassica oleracea) extracts incorporated biosensor for colorimetric detection of Helicobacter pylori with color image processing
Brazilian Journal of Microbiology (2023)
-
Trimer stability of Helicobacter pylori HtrA is regulated by a natural mutation in the protease domain
Medical Microbiology and Immunology (2023)
-
Optical detection using CRISPR-Cas12a of Helicobacter pylori for veterinary applications
Microchimica Acta (2023)
-
The TLR/MyD88 signalling cascade in inflammation and gastric cancer: the immune regulatory network of Helicobacter pylori
Journal of Molecular Medicine (2023)