Abstract
Since 1997, several epizootic avian influenza viruses (AIVs) have been transmitted to humans, causing diseases and even deaths. The recent emergence of severe human infections with AIV (H7N9) in China has raised concerns about efficient interpersonal viral transmission, polygenic traits in viral pathogenicity and the management of newly emerging strains. The symptoms associated with viral infection are different in various AI strains: H5N1 and newly emerged H7N9 induce severe pneumonia and related complications in patients, while some H7 and H9 subtypes cause only conjunctivitis or mild respiratory symptoms. The virulence and tissue tropism of viruses as well as the host responses contribute to the pathogenesis of human AIV infection. Several preventive and therapeutic approaches have been proposed to combat AIV infection, including antiviral drugs such as M2 inhibitors, neuraminidase inhibitors, RNA polymerase inhibitors, attachment inhibitors and signal-transduction inhibitors etc. In this article, we summarize the recent progress in researches on the epidemiology, clinical features, pathogenicity determinants, and available or potential antivirals of AIV.
Similar content being viewed by others
Introduction
Avian influenza virus (AIV) is a potential source for the emergence of human influenza pandemics. Historically, several harmful influenza pandemics have originated from AIVs through genetic reassortment between human and avian influenza strains, as happened in the 1918 H1N1, 1957 H2N2, and 1968 H3N2 pandemics1,2. The unprecedented emergence of H5N1 human infections in 1997 provided the first evidence that AIV could directly transmit from poultry to humans3. Since February 2013, there have been cases of severe human infection with H7N9 AIV in China; this AIV strain consists of genes from three AIV strains and is viewed as a pandemic threat4.
Avian influenza virus (AIV) is an influenza A virus, which is a member of the genus Orthomyxovirus. The genome of AIV consists of eight minus-sense single-stranded RNA segments that encode a minimum of 10 unique viral proteins. The current classification into subtypes is based on the surface glycoproteins hemagglutinin (HA) and neuraminidase (NA). To date, 16 HA subtypes and nine NA subtypes have been described5,6. The unique genome of influenza virus H17N10 was recently discovered in bats in Guatemala7. One remarkable feature of influenza viruses is their inclination to undergo antigenic variation through antigenic drift and antigenic shift8. Antigenic drift consists of relatively minor mutational alterations in the antigenicity of HA or NA and occurs continuously as a result of selection pressure from host immunity8. Antigenic shift by genetic reassortment of the eight gene segments can result in the appearance of a novel HA/NA combination against which the human population has little or no immunity9. If the majority of people are immunologically naïve to novel strains and such strains can be transmitted efficiently from human to human, influenza pandemics may occur9.
Aquatic birds are the reservoirs of all influenza A virus subtypes. Most influenza viruses infect wild and/or domestic birds with limited or no signs of the disease and are thus classified as low pathogenic avian influenza (LPAI) viruses10. However, highly pathogenic avian influenza (HPAI) viruses can cause severe diseases in poultry, with fatality as high as 100%10. Currently, all HPAI viruses belong to subtype H5 or H7, but not all H5 or H7 viruses are HPAI.
Human infections with AIV
Epidemiology
Three different subtypes of AIV have been confirmed as capable of infecting humans: H5, H7, and H9 (Table 1). Humans can be infected by AIV primarily after their mucous membranes have come into direct contact with infectious secretions or excreta from infected birds or contaminated poultry products11. The main infectious route of AIV seems to be via the upper respiratory tract and conjunctivae12,13. Direct introduction to the lower respiratory tract may occur only after massive exposure, such as the culling operations of infected poultries14. The role of infection through other routes (eg, gastrointestinal tract) remains to be explored.
The first warning that AIV could directly transmit from avian species to humans occurred in 1997 in Hong Kong and resulted in 18 infections and 6 deaths3. HPAI H5N1 influenza viruses were found to be endemic in poultry in most provinces of southern China, a fact that was supported by long-term surveillance15,16,17. Since 1997, HPAI H5N1 has spread from Asia to Europe, Africa, and the Far East through the poultry trade and migratory bird movements18,19,20,21,22. More than 600 cases of human infection have been confirmed in the past 10 years, and the fatality rate is approximately 60%23. Children and young adults appear to be more susceptible to the virus24.
The H7 subtypes of AIV have caused multiple cases of human infection since 2002 in Canada, China, Italy, Netherlands, the United States, and the United Kingdom25. In 2003, an HPAI H7N7 virus was found to transmit from ducks to humans; 89 cases of human infection were confirmed, and one patient died from severe pneumonia26. Several other AIV H7 strains, including HPAI H7N3, LPAI H7N3, and LPAI H7N2, have had sporadic outbreaks in recent years resulting in only mild illness in humans12,27,28,29,30,31,32. The latest LPAI H7N9 outbreak in China, however, caused several deaths due to severe pneumonia and related complications4,33,34,35,36. Although all H7 types of AIV are still zoonotic, they may be more likely to develop into interpersonal pandemics because these viruses preferentially bind to α-2,6-linked SA and/or a mammalian adaptation trait on the PB2 protein4,25.
Since 1999, when the first human infection of LPAI H9N2 was detected in Hong Kong, this virus has been infrequently isolated from humans30. The symptoms associated with H9N2 infection are generally mild, and there is no evidence of human-to-human transmission30,31,32.
Clinical features
The main clinical manifestations of AIV infection depend on the viral subtype. Some LPAI (eg, H7N2, H7N3, and H9N2) and HPAI strains (H7N7) only cause asymptomatic or mild symptoms, such as conjunctivitis or uncomplicated influenza-like illness, in humans12,37,38,39,40,41,42. In current human infections with LPAI (H7N9), a typical influenza-like illness (eg, fever and cough) appeared in the early course of the disease. Blood biochemistry tests identified that aspartate aminotransferase (AST), lactate dehydrogenase (LDH), and creatine kinase (CK) levels significantly increased, while white blood cell counts were normal or slightly decreased. Some patients progressed to severe pneumonia followed by acute respiratory distress syndrome (ARDS), and finally died from multi-organ failure4. Interstitial infiltration, lobar infiltration, and collapse/consolidation could be observed in chest radiographs 7 to 13 d after the onset of illness. These clinical features of H7N9 infections were comprehensively described by Gao et al43.
In HPAI H5N1 infection, the onset of disease occurred at a median of 3 to 4 d after exposure. The initial symptoms of disease were also influenza-like. Dyspnea could be observed in 42%–72% of patients, and extra-pulmonary symptoms such as conjunctivitis and gastrointestinal symptoms (eg, abdominal pain, diarrhea, and vomiting) occasionally occurred44,45,46. Other complications included Reye's syndrome and pulmonary hemorrhaging44,47,48. Many patients progressed to severe pneumonia, rapidly developed ARDS 4–13 d after disease onset, and finally died from multi-organ failure. Comparing with survivors of HPAI H5N1 infection, fatal cases were more likely to present with leukopenia, lymphopenia, thrombocytopenia, and elevated levels of AST, LDH, and CK49,50,51,52,53. Abnormal chest radiographic findings were the same as those for H7N946.
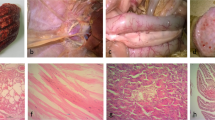
The primary histopathological findings in fatal H5N1 human infections were extensive infiltration of lungs, disseminated intravascular coagulation, and multi-organ failure. In the lung, pneumocytes were the primary target of H5N1 infection, resulting in diffuse alveolar damage with interstitial fibrosis, hyaline membrane formation, patchy interstitial lymphoplasmacytic infiltrates, bronchiolitis with squamous metaplasia, and pulmonary congestion with varying degrees of hemorrhage54,55,56,57. The HPAI (H5N1) virus also infected multiple organs in addition to the lungs. Postmortem findings for patients who died from A/H5N1 infection showed edemas, degeneration of myocytes in the heart, extensive hepatic central lobular necrosis, extensive acute tubular necrosis in the kidney, disseminated intravascular coagulation, and cerebral involvement50,54,58,59,60. A fatal case of AIV (H5N1) infection in a pregnant woman revealed viral infection in the brain, placenta, and fetus55,61. In addition, systemic cytokine activation resulted in hemophagocytic syndrome, lymphoid depletion, and skeletal muscle fiber necrosis54,56.
The viral load of AIV varies in respiratory secretions, tissues, plasma, cerebrospinal fluid, and feces. Respiratory secretions and tissues commonly have the highest viral loads, and virus can be detected in all patients. Infectious virus and viral RNA have been detected in feces and intestines, suggesting that the virus sometimes replicates in the gastrointestinal tract49,59,62. Intestinal involvement in A/H5N1 virus infections may explain the common occurrence of diarrhea. Viral RNA in plasma is more often detected in patients with fatal disease than in those with nonfatal disease, indicating that levels of viral replication may influence the outcome63. A high viral load is also correlated with an increase in host response, as patients with HPAI (H5N1) infections rarely have detectable viral RNA in the respiratory tract for more than 3 weeks63.
Host responses
The severe disease associated with AIV infection in humans could be caused by a variety of mechanisms, including viral dissemination, differences in tissue tropism and host response64. Generally, the host responses to AIV are complicated and include apoptosis and autophagy as well as immune responses (innate, humoral, and cell-mediated)65,66,67,68.
Autophagy, a tightly regulated homeostatic process for self-digestion of unwanted cellular subcomponents, has been suggested to be responsible for lung injury in AIV infection65,66,67. The autophagic death of alveolar epithelial cells may also be responsible for the high mortality rate of H5N1 infection because autophagy-blocking agents applied prophylactically or therapeutically in mice significantly increased the survival rate and alleviated the lung injury caused by H5N1 infection67.
Accumulating evidence suggests that virus-induced cytokine/chemokine dysregulation also plays a significant role in the pathogenesis of AIV infection68. Respiratory epithelial cells and macrophages are the primary innate immune cells involved in AIV infection68. Pronounced activation of the proinflammatory cytokine/chemokine cascade prolongs the period of inflammatory response and contributes to further tissue damage and the persistence of the systemic inflammatory response syndrome69. Furthermore, cytokines can further sensitize neighboring cells by up-regulating RIG-I and amplifying the cytokine cascade in some HPAI infections70. It appears that cytokine responses may be driven by high-level viral replication, because plasma levels of macrophage- and neutrophil-attractant chemokines as well as pro- and anti-inflammatory cytokines (IL-6 and IL-10) were higher in patients with HPAI (H5N1) infection compared to the levels in patients with a conventional influenza infection50.
It should be noted that IL-17, Th-17 mediators, and IL-17-responsive cytokines were found in serum samples of 2009 swine-origin H1N1 influenza virus (S-OIV H1N1) infected patients71. IL-17 deficiency or treatment with monoclonal antibodies can significantly alleviate acute lung injury induced by the S-OIV H1N1 virus in mice71. In addition, IL-17 has been suggested to enhance the proinflammatory outcome of an antiviral response in human cells72. Thus, monoclonal antibodies against IL-17 may be helpful to reduce severe lung injury induced by AIV infections.
The suppression of interferon is also involved in human AIV infection. HPAI (H5N1) was found to attenuate the expression of IRF3 as well as the levels of type I IFNs, and subsequently substantially delay the phosphorylation of Stat2 and induction of IFN-stimulated genes (ISGs) in vitro73,74. Viral protein M2 appeared to be the “main culprit” that correlated with the complete suppression of known viral inflammasome activation75.
In addition to cytokine response, apoptosis and autophagy, other humoral and cell immune responses are also involved in AIV infection68,76. Surprisingly, although some of these responses exhibited antiviral activity, they did not affect virus replication, although some immune cells cannot be excluded from playing a role in the dissemination of the virus in vivo60,68.
Pathogenicity determinants
The virulence of AIV is determined by a constellation of genes77,78,79,80,81. These genes play important roles in viral replication and/or pathogenicity and are also potential targets of antiviral agents.
HA protein
HA influenza virus protein plays a crucial role in the early stages of the viral life cycle by binding to the viral receptor and mediating the fusion process11. Influenza virus infection begins when HA binds to sialic acid (SA)-linked glycoprotein receptors on the surface of the target cell. Usually, AIVs preferentially bind to α-2,3 linked SA, which is located mainly on type II pneumocytes, alveolar macrophages and nonciliated cuboidal epithelial cells at terminal bronchioles, while human influenza viruses tend to use α-2,6 linked SA as a receptor in the upper respiratory tract of humans11,82,83,84,85. AIVs can infect human airway epithelium, but replication is limited due to the non-optimal cellular tropism86. Thus, the adaptation of AIV HA for recognition of α-2,6 linked SA located in the human upper respiratory tract would promote interpersonal transmission. Amino acids in the HA receptor-binding domain (RBD), formed by the 190-helix, 220-loop, and 130-loop, determine the receptor binding preference of influenza viruses87,88,89. However, several AIV (H5N1) strains with increased binding to human-type receptors isolated from humans still prefer binding to avian-type receptors and do not perform efficient human-to-human transmission90,91,92,93,94. An LPAI (H7N2) strain isolated from humans has also been reported to have dual binding affinity to both types of receptors, but no obvious inter-personal or inter-mammalian transmission was observed95. The H7N2 strain has an eight amino acid deletion in the 220-loop of the HA RBD95. Two specific mutations in H7-HA, Q226L and G228S, have also been suggested to contribute to the increased binding affinity for human receptors96. The Q226L mutation was identified in clinical isolates of H7N9 in 20134. Five amino acid substitutions (or four with reassortment) in HA of the H5N1 virus have efficiently supported airborne viral transmission among mammals97,98,99.
The post-translational cleavage of HA0 into HA1 and HA2 subunits activates the membrane fusion potential of HA and is crucial for infectivity of the virus100. Most LPAI viruses possess a single arginine residue at the cleavage site of HA, which is cleaved by extracellular trypsin-like proteases restricted to the respiratory tract101. In contrast, HPAI viruses contain a motif of multiple basic amino acid residues at the equivalent cleavage site, permitting HA0 to be cleaved by ubiquitously distributed intracellular proteases, such as furin-like proteases, and enabling systemic infection100,102,103,104. Notably, the circulating H7N9 virus possesses only a single arginine at the HA cleavage site, yet it has caused severe disease and death in humans4,34. This fact indicates that the existence of a multibasic cleavage site is not essential for the high pathogenicity of AIV in humans and other genes may also be involved. A flexible loop structure in the cleavage site between HA1 and HA2 is critical for the efficient cleavage of HA0. The relatively stable alpha-helix structure in the flexible cleavage loop (eg, key residue R328 hidden behind the helix) and the inaccessibility of the cleavage site may contribute to the low pathogenicity of a H16 subtype AIV105. The natural alpha-helix element might also provide a new opportunity for influenza virus inhibitor design105.
NA protein
An evolutionary balance between the HA and NA proteins of AIVs is essential for the entry and release processes of the virus106. As a result, mutations within the active sites of either HA or NA can affect the enzymatic activity of both proteins. For example, some H5N1 viruses in sustained circulation in poultry possess additional glycosylation sites and a shortened NA stalk, both of which might enhance the virulence of AIV in mammals107. A deletion of five amino acids in the NA stalk region was also found in circulating H7N9 isolates4, which may help to explain the unusually high virulence of this strain.
Ribonucleoprotein complex (RNP)
The polymerases PB2, PB1, and PA, and the nucleocapsid protein (NP) together form the RNP, which is critical for virus replication, virulence, and the determination of host restrictions108. Several amino acids in PB1 (eg, positions 99 and 368) and PB2 (eg, positions 89, 627, and 701) are basic molecular determinants associated with enhancing polymerase activity and pathogenicity of H5N1 virus in mammals109. Mutations of these positions in the H5N1 virus can not only promote higher viral yields in both the upper and lower respiratory tract of mice but also result in the conversion of a non-lethal H5N1 virus to a lethal one110. Similar mutations can also be observed in the currently circulating H7N9 virus4,34,36,111,112.
PB1-F2 protein
Produced by an alternate reading frame in the PB1 gene, PB1-F2 is a non-structural accessory protein in influenza A viruses113. PB1-F2 protein is expressed by almost all avian influenza A strains, but strains from human and swine hosts have forms with premature truncations at either the C- or N- terminal end114,115.
PB1-F2 has been shown to specifically target and sensitize alveolar macrophages to apoptotic stimuli116,117. The presence of an intact PB1-F2 protein was also found to contribute to viral pathogenicity; an N66S mutation in H5N1 PB1-F2 led to the delayed activation of IFN-stimulated genes and increased cytokine/chemokine levels in mice due to the inhibition of early type I IFN responses at the level of the mitochondrial antiviral signaling protein (MAVS)118,119.
The precise function of the PB1-F2 protein remains unclear. Research on this protein has indicated that the PB1-F2 protein has strain-specific functions that could vary in different hosts120,121.
NS1 protein
A multi-functional nonstructural RNA-binding protein, NS1 is critical for inhibiting both IFN production and the antiviral effects of IFN-induced proteins, such as dsRNA-dependent protein kinase R (PKR) and RNase L122,123. A P42S mutation in NS1 dramatically increased the virulence of an H5N1 strain in mice and was also found in the circulating H7N9 virus4,124. This substitution, in association with other mutations in HA, NA, PB1, and PB2, contribute to the pathogenicity of AIV H7N9 in humans.
Antiviral agents against AIV
Several safe and effective drugs can be used to manage human and avian influenza infection. These agents include M2, neuraminidase, polymerase, attachment and signal-transduction inhibitors as well as ribavirin, arbidol, and herbs. Several M2 and neuraminidase inhibitors have been approved for prophylaxis and the therapeutic treatment of influenza (Table 2). Other agents are still being studied in preclinical or clinical investigations. Here, we review the basic pharmacokinetics and properties that support the use of these agents against AIV.
M2 inhibitors
The migration of H+ ions into the interior of viral particles is mediated by the M2 channel and allows for the uncoating of virus particles in the endosome125,126. There are two commercially available M2 inhibitors: amantadine and rimantadine (Table 2). They have been widely used in the treatment of both human and avian influenza infections for many years and have been shown to shorten the disease duration and facilitate symptom resolution127.
Unfortunately, most of the currently circulating animal viruses, including H5N1, H9N2, the 2009 swine-originated H1N1, and current H7N9, are all M2 inhibitor resistant due to overuse of the inhibitors111,128,129,130. The widespread resistance of these strains precludes the use of these M2 inhibitors in most cases of human infection131,132. Resistance mutations occur mainly in the trans-membrane portion of the M2 protein (position 26, 27, 30, 31, or 34) and result in an enlarged diameter of the M2 channel pore, thus reducing the binding of M2 inhibitors126. Different subtypes or clades of AIV exhibit different frequencies of M2 inhibitor resistance133. For example, all 24 cases of clade 1 H5N1 isolated between 2008–2011 had an S31N substitution, while the frequency of this mutation in clade 2 ranged from 0% to 67%. In addition, all 3 cases of H7N9 that have been isolated are S31N variations133. It seems that the increase in adamantane-resistant influenza viruses is not mediated by continued selective drug pressure; therefore, the WHO recommends amantadine or rimantadine only be used to prevent or treat AIV that is known to be sensitive. Interestingly, one study suggested that a G23C mutation in the H7 HA protein might also play a role in amantadine resistance134. In addition, several novel M2 inhibitors, including new adamantane derivatives and biological agents (eg, annexin A6), have shown marked activity against human influenza viruses135,136,137. Whether any of these agents could replace amantadine and rimantadine as an influenza virus treatment needs to be further explored.
Neuraminidase inhibitors
Viral neuraminidase (NA) enables progeny virus to be cleaved from its receptor and spread to other cells. The neuraminidase inhibitors, which are cyclopentane or pyrrolidine derivatives, can prevent the further spread of influenza by blocking the release of newly formed particles138. Four commercial neuraminidase inhibitors (oseltamivir, zanamivir, peramivir, and laninamivir) have been approved for use in humans139. The first two are widely used in most countries and are effective against influenza infection. Particularly for oseltamivir, early administration can not only shorten the duration of illness but also facilitate symptom resolution139. Neuraminidase inhibitors are also effective against different AIV subtypes in vitro (Table 2)140,141,142. Studies in animal models have demonstrated that oseltamivir given as treatment or prophylaxis was active against the H5, H7, and H9 avian influenza strains140,143. The protective efficacy was influenced by the virulence of the strains, the dosage and treatment initiation time140,143. Clinical trials also suggested that oseltamivir and zanamivir were useful in reducing the mortality of lethal H5N1 infection, while resistance to the treatments rarely emerged132. Therefore, the WHO recommends these two agents as the primary intervention for treatment and prevention of human AIV infections. However, continued monitoring of AIV for drug susceptibility is needed, because oseltamivir-resistant seasonal influenza strains have been spreading around the world since 2009144,145. Notably, one of the current H7N9 isolates has an R292K substitution4, which has been associated with in vitro resistance to neuraminidase inhibitors in another N9 NA subtype AIV. This mutation has also been confirmed to lead to oseltamivir- and zanamivir-resistance in clinical N2 AIV subtype (Table 3)146. The presence of the NA R292K substitution in two H7N9 patients who also received corticosteroid treatment resulted in treatment failure147. Thus, it is crucial to assess the prevalence of drug-resistant H7N9 in future influenza surveillance. Among the newly developed neuraminidase inhibitors, laninamivir has an extremely long persistence time in the lungs141, increasing the prospect of a long-lasting antiviral that can effectively prevent influenza infection with a single dose.
RNA polymerase inhibitors
The influenza polymerase consists of several polypeptides, including PB1, PB2, and PA, and also contributes to the high virulence of AIV in humans1,4,148. Therefore, novel antivirals that target polymerase are anticipated to reduce the replication of AIV as well as inhibit the severe pathogenicity induced by the virus. Current influenza RNA polymerase inhibitors can be divided into nucleosides and non-nucleosides. These polymerase inhibitors, such as fluorodeoxycytidine analogs and favipiravir (T705), have been shown to be active in the treatment of influenza both in vitro and in vivo149,150,151. The most potent inhibitor among fluorodeoxycytidine analogs was 2′-deoxy-2′-fluorocytidine (2′-FdC) which inhibited various strains of HPAI and LPAI with 50% inhibitory concentrations (IC50s) ranging from 0.21 to 3.2 μmol/L in MDCK cells149. 2′-FdC 60 mg·kg−1·d−1 of (ip, bid×8 d) could protect 60%–80% of mice from lethal HPAI H5N1 infection when administered 24 h before virus exposure149. T705 is a pro-drug that needs to be converted to its active form, T705-RTP150. T705-RTP then competitively inhibits the RNA synthesis activity of influenza polymerase. T705 was effective against several H5N1 strains with an IC50 range of 1.3–7.7 μmol/L in vitro, while the range of oseltamivir was 0.007–0.92 μmol/L151. In vivo, T705 300 mg·kg−1·d−1 with different delivery methods was able to protect 100% of mice from a lethal H5N1 infection151.
Several other polymerase inhibitors are in development against AIV infection. A GTPase induced by type I and type III IFNs, Mx1, inhibits influenza virus infection by interacting with the ribonucleoprotein complex and interfering with viral assembly by disrupting the PB2-NP interaction152. A short peptide derived from PB1 (731–757) was also reported to inhibit virus polymerase153. Several small interfering RNAs (siRNAs) targeting the overlapping gene of PB1 and PB1-F2 were found to reduce virus-associated cell apoptosis and virus titers in chicken embryos154. A novel compound, THC19, inhibited influenza viral genome replication and/or transcription in a PA-dependent manner155. Another novel compound, ASN2, induced IFN production and inhibited growth of influenza A viruses through ASN2-mediated inhibition of viral polymerase function and the subsequent loss of expression of the viral IFN antagonist, NS1156.
Although the efficacy of these polymerase inhibitors needs to be further examined in clinical investigations, these leading compounds have resulted in the development of a series of novel anti-influenza agents that target the viral RNA polymerase.
Ribavirin and arbidol
Ribavirin and arbidol have long been recognized as broad-spectrum antiviral agents against viruses from different families. Viruses resistant to these treatments have rarely been observed157,158,159,160,161,162. The target of ribavirin is a cellular enzyme, inosine 5′-monophosphate (IMP) dehydrogenase, which is involved in viral RNA synthesis and cellular biosynthesis of GTP. The IC50 of ribavirin on H5N1 ranged from 6 to 22 μmol/L in vitro157. Ribavirin 75 mg·kg−1·d−1 (po, bid×8 d) protected 70% of mice from lethal H5N1 infection163. The clinical efficacy of ribavirin on influenza was less effective than that of adamantanes or NA inhibitors and more dependent on the delivery manner162,164,165. Aerosolized ribavirin effectively eliminated the influenza virus and shortened the duration of illness in clinical observations, while orally administered ribavirin did not162,164,165. However, the clinical utility of ribavirin may be limited due to the risk of hemolytic anemia and teratogenicity166. A prodrug of ribavirin, viramidine, may improve the utility of ribavirin157. This prodrug had a similar activity against seasonal and H5N1 influenza viruses but was less toxic. Furthermore, viramidine effectively protected mice from lethal influenza, even when the drug was administered in drinking water157. This drug is now in Phase 3 development for HCV treatment167.
Arbidol has been widely used in Russia for almost 20 years158. The mechanisms of arbidol are complicated; both membrane fusion inhibition and immunomodulatory activity may contribute to its broad antiviral effects158. Arbidol was shown to stabilize HA by causing a 0.2 pH unit reduction in the pH required for transition to the low pH form of the protein. A recombinant arbidol-resistant strain possessed single amino acid substitutions in the HA2 subunit that abrogated this activity of arbidol168. Arbidol was active against H5N1, H9N2, H2N2, and H6N1 AIV with a range of IC50 values from 19.4 to 58.3 μmol/L160,169. Our current research also confirmed that post-treatment with arbidol decreased the mortality in influenza-infected mice by mitigating lung lesion formation and reducing viral titers170. Furthermore, it efficiently protected the host from virus-induced inflammation by modulating the expression of pro-inflammatory cytokines170. These data suggest that arbidol might also be effective in the treatment of severe AIV infections in humans.
Attachment inhibitors
As mentioned above, influenza virus needs to attach the SA receptor to enter host cells. A number of attachment inhibitors have been developed against AIV, including sialidase mimics, sialyl glycopolymers and hemagglutinin inhibitors. The sialidase recombinant construct DAS181 is an inhaled bacterial sialidase that prevents the attachment and subsequent infection of influenza virus by removing influenza-receptor interactions171. DAS181 was shown to have activity against H5N1 infection in both continuous and shorter treatments in human airway epithelium models172. Further studies were performed in lethally H5N1-infected mice models; 1 mg·kg−1·d−1 DAS181 (inhale, qd×8 d) protected 100% of mice from viral infection in both prophylactic and therapeutic approaches173,174. A phase 2 study of DAS181 on seasonal or pandemic influenza has been completed, and when patients were given 10 mg·kg−1·d−1 DAS181 (inhale, qd×3 d), they showed a significant reduction in viral load over 5 d, but no symptom improvement175. Sialylglycopolymers and other hemagglutinin inhibitors (eg, Neo6, EB peptide, and NDFRSKT peptide) showed enhanced binding affinity for HA compared to normal SA, allowing them to block attachment of H5N1 and H9N2 AIV176,177,178,179,180. A fusion inhibitor, tert-butyl hydroquinone (TBHQ), bound in a hydrophobic pocket formed at the interface between HA monomers and consequently inhibited the conformational rearrangements required for membrane fusion181. Although most of these agents are still in pre-clinical studies, they are anticipated to be used against any newly emerging influenza strains, especially AIV178,179.
Signal-transduction inhibitors
Aside from agents that directly target viral proteins, current antiviral strategies also focus on the intracellular cascade needed for viral replication182,183,184. Two signaling pathways that are required to ensure efficient virus replication have been considered suitable targets for antiviral approaches: the IKK/NF-κB module and the Raf/MEK/ERK cascade184. Both of these pathways are also critical for cytokine and interferon synthesis during influenza infection182,183,184. Thus, inhibitors targeting these cascades may not only inhibit the replication of virus but also moderate the severe systemic inflammation in AIV infection184. This hypothesis has been confirmed by several laboratory experiments in vitro and in vivo182,183,184,185, although the efficacy in humans needs to be further investigated. However, some inhibitors targeting NF-κB, such as aspirin, have been routinely used in influenza-like illness for many years185. Current research identified that a high dosage of aspirin efficiently blocked influenza virus replication both in vitro and in vivo, and there are plans to use this drug in clinical studies with administration via inhalation185. Several other anti-inflammatory agents (eg, statins and sphingosine analogs) have also received attention and are being investigated186,187,188,189,190. However, results from these studies were mixed and sometimes even conflict186,187,188,189,190. Nonetheless, these studies have promoted optimization of these agents and suggested new strategies for therapies against AIV infection.
Herbs
Herbs may also be a potential choice for AIV treatment. Some Chinese herbs were recommended and authorized by the Chinese government during the 2009 H1N1 and 2013 H7N9 pandemics191,192. Herbal medicines that contain Isatis tinctoria L, Lonicera japonica Thunb, Saposhnikovia divaricata (Turcz) Schischk, Bupleurum chinense DC, Forsythia suspensa (Thunb) Vahl, Citrus reticulata Blanco, and Perilla frutescens (L) Britton are commonly taken in a formula used for the prophylactic and therapeutic treatment of influenza infection. A number of clinical trials for these herbs for the treatment of influenza have been conducted, but systematic reviews on the utility of these herbs for H1N1 influenza treatment have revealed that few herbal medicines showed a positive effect on viral shedding, and most of the medicines had a positive effect only on fever resolution or relief of symptoms193,194. Although more rigorous placebo-controlled and randomized trials are needed to reach further conclusions193,194, many Chinese herbs exhibit beneficial immunomodulatory effects for rapid recovery of viral infections and might be effective treatments for AIV infection195.
Other emerging agents
Recently, several active proteases of influenza A viruses such as TMPRSS2 (transmembrane protease serine S1 member 2) and HAT (human airway trypsin-like protease) have been considered potential drug targets. Peptide mimetic protease inhibitors (eg, BAPA) suppressed the cleavage activation of HA and the spread of virus in TMPRSS2- and HAT-expressing cells196,197.
Serine proteases, which mediate influenza HA cleavage, are responsible for influenza virus activation. Agents targeted to serine proteases (eg, aprotinin, leupeptin, and camostat) suppressed the cleavage of HA and limited the reproduction of human and avian influenza viruses that have a single arginine in the HA cleavage site. It is anticipated that these agents will be used for the treatment of HPAI viruses (eg, H5 and H7), whose hemagglutinins possess multi-arginine/lysine cleavage sites198.
There are also several compounds that target the NS1 protein and show considerable anti-influenza potential. For example, JJ3297 inhibits the replication and spread of influenza virus by reversing the NS1-induced inhibition of interferon mRNA production in an RNase L-dependent manner199. A C-Jun N-terminal kinase (JNK) inhibitor, SP600125, reduced the amplification of influenza virus by indirectly inhibiting the NS1-mediated supportive functions200.
Conclusion
Persistent outbreaks of avian influenza in Southeast Asia suggest that avian influenza may be the most likely candidate for the next influenza pandemic. Many AIV patients died from overwhelming viral pneumonia with other serious complications. Thus, rapid, sensitive, and confirmatory diagnoses for early identification and continued monitoring of viral adaptation to humans are essential for the control of AIV infections. It should be noted that AIV infections differ from human influenza infections in humans in many ways, including viral transmission, viral dissemination, clinical features, pathogenesis, and host response. The diagnosis and therapy of AIV infections have unique features as well. For example, sample analysis from the lower respiratory tract may offer a more sensitive diagnosis. Several drugs have been used as prophylactic or therapeutic treatments against AIV infection, including M2 inhibitors, neuraminidase inhibitors, ribavirin, etc. As the frequency of drug-resistant influenza increases, the rational use of antivirals, and drug-resistant monitoring should be encouraged. Meanwhile, efforts should be made to design and develop further new antivirals that target the basic steps of viral replication, such as attachment, internalization, and cellular processes, or relatively specific targets, such as the viral RNA polymerase, PB1-F2, NS1, etc.
References
de Wit E, Fouchier RA . Emerging influenza. J Clin Virol 2008; 41: 1–6.
Smith GJ, Bahl J, Vijaykrishna D, Zhang J, Poon LL, Chen H, et al. Dating the emergence of pandemic influenza viruses. Proc Natl Acad Sci U S A 2009; 106: 11709–12.
Shortridge KF, Zhou NN, Guan Y, Gao P, Ito T, Kawaoka Y, et al. Characterization of avian H5N1 influenza viruses from poultry in Hong Kong. Virology 1998; 252: 331–42.
Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, et al. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med 2013; 368: 1888–97.
Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y . Evolution and ecology of influenza A viruses. Microbiol Rev 1992; 56: 152–79.
Swayne DE, Suarez DL . Highly pathogenic avian influenza. Rev Sci Tech 2000; 19: 463–82.
Tong S, Li Y, Rivailler P, Conrardy C, Castillo DA, Chen LM, et al. A distinct lineage of influenza A virus from bats. Proc Natl Acad Sci U S A 2012; 109: 4269–74.
Shoham D . The modes of evolutionary emergence of primal and late pandemic influenza virus strains from viral reservoir in animals: an interdisciplinary analysis. Influenza Res Treat 2011; 2011: 861792.
Taubenberger JK, Morens DM . Influenza: the once and future pandemic. Public Health Rep 2010; 125 Suppl 3: 16–26.
Barratt-Boyes SM . Comparative immunology, microbiology and infectious diseases. Introduction. Comp Immunol Microbiol Infect Dis 2012; 35: 217–8.
Yin J, Liu S, Zhu Y . An overview of the highly pathogenic H5N1 influenza virus. Virol Sin 2013; 28: 3–15.
Hirst M, Astell CR, Griffith M, Coughlin SM, Moksa M, Zeng T, et al. Novel avian influenza H7N3 strain outbreak, British Columbia. Emerg Infect Dis 2004; 10: 2192–5.
Kurtz J, Manvell RJ, Banks J . Avian influenza virus isolated from a woman with conjunctivitis. Lancet 1996; 348: 901–2.
Wong SS, Yuen KY . Avian influenza virus infections in humans. Chest 2006; 129: 156–68.
Chen H, Smith GJ, Li KS, Wang J, Fan XH, Rayner JM, et al. Establishment of multiple sublineages of H5N1 influenza virus in Asia: implications for pandemic control. Proc Natl Acad Sci U S A 2006; 103: 2845–50.
Smith GJ, Fan XH, Wang J, Li KS, Qin K, Zhang JX, et al. Emergence and predominance of an H5N1 influenza variant in China. Proc Natl Acad Sci U S A 2006; 103: 16936–41.
Wang J, Vijaykrishna D, Duan L, Bahl J, Zhang JX, Webster RG, et al. Identification of the progenitors of Indonesian and Vietnamese avian influenza A (H5N1) viruses from southern China. J Virol 2008; 82: 3405–14.
Lee CW, Suarez DL, Tumpey TM, Sung HW, Kwon YK, Lee YJ, et al. Characterization of highly pathogenic H5N1 avian influenza A viruses isolated from South Korea. J Virol 2005; 79: 3692–702.
Mase M, Tsukamoto K, Imada T, Imai K, Tanimura N, Nakamura K, et al. Characterization of H5N1 influenza A viruses isolated during the 2003–2004 influenza outbreaks in Japan. Virology 2005; 332: 167–76.
Nguyen DC, Uyeki TM, Jadhao S, Maines T, Shaw M, Matsuoka Y, et al. Isolation and characterization of avian influenza viruses, including highly pathogenic H5N1, from poultry in live bird markets in Hanoi, Vietnam, in 2001. J Virol 2005; 79: 4201–12.
Al-Azemi A, Bahl J, Al-Zenki S, Al-Shayji Y, Al-Amad S, Chen H, et al. Avian influenza A virus (H5N1) outbreaks, Kuwait, 2007. Emerg Infect Dis 2008; 14: 958–61.
Perk S, Banet–Noach C, Golender N, Simanov L, Rozenblut E, Nagar S, et al. Molecular characterization of the glycoprotein genes of H5N1 influenza A viruses isolated in Israel and the Gaza Strip during 2006 outbreaks. Virus Genes 2007; 35: 497–502.
Weekly epidemiological record. ed: WHO 2013: 137–44.
Yee KS, Carpenter TE, Cardona CJ . Epidemiology of H5N1 avian influenza. Comp Immunol Microbiol Infect Dis 2009; 32: 325–40.
Belser JA, Bridges CB, Katz JM, Tumpey TM . Past, present, and possible future human infection with influenza virus A subtype H7. Emerg Infect Dis 2009; 15: 859–65.
Koopmans M, Wilbrink B, Conyn M, Natrop G, van der Nat H, Vennema H, et al. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 2004; 363: 587–93.
Avian influenza A/(H7N2) outbreak in the United Kingdom. Euro Surveill 2007; 12: E070531 2.
CDC. Update: influenza activity — United States and worldwide, 2003–04 season, and composition of the 2004–05 influenza vaccine. MMWR Morb Morta Wkly Rep 2004; 53: 547–52.
CDC. Update: influenza activity — United States and worldwide, 2002–03 season, and composition of the 2003–04 influenza vaccine. MMWR Morb Morta Wkly Rep 2003; 52: 516–21.
Peiris M, Yam WC, Chan KH, Ghose P, Shortridge KF . Influenza A H9N2: aspects of laboratory diagnosis. J Clin Microbiol 1999; 37: 3426–7.
Butt AM, Siddique S, Idrees M, Tong Y . Avian influenza A (H9N2): computational molecular analysis and phylogenetic characterization of viral surface proteins isolated between 1997 and 2009 from the human population. Virol J 2010; 7: 319.
WHO. Weekly epidemiological record. WHO 2011: 469–80.
Li Q, Zhou L, Zhou M, Chen Z, Li F, Wu H, et al. Preliminary report: epidemiology of the avian influenza A (H7N9) outbreak in China. N Engl J Med 2013. doi: 10.1056/NEJMoa1304617.
Chen Y, Liang W, Yang S, Wu N, Gao H, Sheng J, et al. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet 2013; 381: 1916–25.
WHO. Number of confirmed human cases for avian influenza A(H7N9) reported to WHO [undated 2013 May 30]. Available from: http://www.who.int/influenza/human_animal_interface/influenza_h7n9/Data_Reports/en/index.html.
Li J, Yu X, Pu X, Xie L, Sun Y, Xiao H, et al. Environmental connections of novel avian-origin H7N9 influenza virus infection and virus adaptation to the human. Sci China Life Sci 2013; 56: 485–92.
Tweed SA, Skowronski DM, David ST, Larder A, Petric M, Lees W, et al. Human illness from avian influenza H7N3, British Columbia. Emerg Infect Dis 2004; 10: 2196–9.
Nguyen-Van-Tam JS, Nair P, Acheson P, Baker A, Barker M, Bracebridge S, et al. Outbreak of low pathogenicity H7N3 avian influenza in UK, including associated case of human conjunctivitis. Euro Surveill 2006; 11: E060504 2.
Ostrowsky B, Huang A, Terry W, Anton D, Brunagel B, Traynor L, et al. Low pathogenic avian influenza A (H7N2) virus infection in immunocompromised adult, New York, USA, 2003. Emerg Infect Dis 2012; 18: 1128–31.
Arzey GG, Kirkland PD, Arzey KE, Frost M, Maywood P, Conaty S, et al. Influenza virus A (H10N7) in chickens and poultry abattoir workers, Australia. Emerg Infect Dis 2012; 18: 814–6.
Butt KM, Smith GJ, Chen H, Zhang LJ, Leung YH, Xu KM, et al. Human infection with an avian H9N2 influenza A virus in Hong Kong in 2003. J Clin Microbiol 2005; 43: 5760–7.
Lin YP, Shaw M, Gregory V, Cameron K, Lim W, Klimov A, et al. Avian-to-human transmission of H9N2 subtype influenza A viruses: relationship between H9N2 and H5N1 human isolates. Proc Natl Acad Sci U S A 2000; 97: 9654–8.
Gao HN, Lu HZ, Cao B, Du B, Shang H, Gan JH, et al. Clinical findings in 111 cases of influenza A (H7N9) virus infection. N Engl J Med 2013; 368: 2277–85.
Yuen KY, Chan PK, Peiris M, Tsang DN, Que TL, Shortridge KF, et al. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet 1998; 351: 467–71.
Chan PK . Outbreak of avian influenza A (H5N1) virus infection in Hong Kong in 1997. Clin Infect Dis 2002; 34 Suppl 2: S58–64.
Liem NT, Tung CV, Hien ND, Hien TT, Chau NQ, Long HT, et al. Clinical features of human influenza A (H5N1) infection in Vietnam: 2004–2006. Clin Infect Dis 2009; 48: 1639–46.
Ku AS, Chan LT . The first case of H5N1 avian influenza infection in a human with complications of adult respiratory distress syndrome and Reye's syndrome. J Paediatr Child Health 1999; 35: 207–9.
Korteweg C, Gu J . Pathology, molecular biology, and pathogenesis of avian influenza A (H5N1) infection in humans. Am J Pathol 2008; 172: 1155–70.
Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, et al. Avian influenza A (H5N1) infection in humans. N Engl J Med 2005; 353: 1374–85.
de Jong MD, Simmons CP, Thanh TT, Hien VM, Smith GJ, Chau TN, et al. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat Med 2006; 12: 1203–7.
Oner AF, Bay A, Arslan S, Akdeniz H, Sahin HA, Cesur Y, et al. Avian influenza A (H5N1) infection in eastern Turkey in 2006. N Engl J Med 2006; 355: 2179–85.
Buchy P, Mardy S, Vong S, Toyoda T, Aubin JT, Miller M, et al. Influenza A/H5N1 virus infection in humans in Cambodia. J Clin Virol 2007; 39: 164–8.
Shinde V, Hanshaoworakul W, Simmerman JM, Narueponjirakul U, Sanasuttipun W, Kaewchana S, et al. A comparison of clinical and epidemiological characteristics of fatal human infections with H5N1 and human influenza viruses in Thailand, 2004–2006. PLoS One 2011; 6: e14809.
To KF, Chan PK, Chan KF, Lee WK, Lam WY, Wong KF, et al. Pathology of fatal human infection associated with avian influenza A H5N1 virus. J Med Virol 2001; 63: 242–6.
Gu J, Xie Z, Gao Z, Liu J, Korteweg C, Ye J, et al. H5N1 infection of the respiratory tract and beyond: a molecular pathology study. Lancet 2007; 370: 1137–45.
Ng WF, To KF, Lam WW, Ng TK, Lee KC . The comparative pathology of severe acute respiratory syndrome and avian influenza A subtype H5N1 — a review. Hum Pathol 2006; 37: 381–90.
Uiprasertkul M, Kitphati R, Puthavathana P, Kriwong R, Kongchanagul A, Ungchusak K, et al. Apoptosis and pathogenesis of avian influenza A (H5N1) virus in humans. Emerg Infect Dis 2007; 13: 708–12.
Chokephaibulkit K, Uiprasertkul M, Puthavathana P, Chearskul P, Auewarakul P, Dowell SF, et al. A child with avian influenza A (H5N1) infection. Pediatr Infect Dis J 2005; 24: 162–6.
Uiprasertkul M, Puthavathana P, Sangsiriwut K, Pooruk P, Srisook K, Peiris M, et al. Influenza A H5N1 replication sites in humans. Emerg Infect Dis 2005; 11: 1036–41.
Gao R, Dong L, Dong J, Wen L, Zhang Y, Yu H, et al. A systematic molecular pathology study of a laboratory confirmed H5N1 human case. PLoS One 2010; 5: e13315.
Shu Y, Yu H, Li D . Lethal avian influenza A (H5N1) infection in a pregnant woman in Anhui Province, China. N Engl J Med 2006; 354: 1421–2.
de Jong MD, Bach VC, Phan TQ, Vo MH, Tran TT, Nguyen BH, et al. Fatal avian influenza A (H5N1) in a child presenting with diarrhea followed by coma. N Engl J Med 2005; 352: 686–91.
Abdel-Ghafar AN, Chotpitayasunondh T, Gao Z, Hayden FG, Nguyen DH, de Jong MD, et al. Update on avian influenza A (H5N1) virus infection in humans. N Engl J Med 2008; 358: 261–73.
Peiris JS, Cheung CY, Leung CY, Nicholls JM . Innate immune responses to influenza A H5N1: friend or foe? Trends Immunol 2009; 30: 574–84.
Law AH, Lee DC, Yuen KY, Peiris M, Lau AS . Cellular response to influenza virus infection: a potential role for autophagy in CXCL10 and interferon-alpha induction. Cell Mol Immunol 2010; 7: 263–70.
Ma J, Sun Q, Mi R, Zhang H . Avian influenza A virus H5N1 causes autophagy-mediated cell death through suppression of mTOR signaling. J Genet Genomics 2011; 38: 533–7.
Sun Y, Li C, Shu Y, Ju X, Zou Z, Wang H, et al. Inhibition of autophagy ameliorates acute lung injury caused by avian influenza A H5N1 infection. Sci Signal 2012; 5: ra16.
Peiris JS, de Jong MD, Guan Y . Avian influenza virus (H5N1): a threat to human health. Clin Microbiol Rev 2007; 20: 243–67.
Cheung CY, Poon LL, Lau AS, Luk W, Lau YL, Shortridge KF, et al. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet 2002; 360: 1831–7.
Hui KP, Lee SM, Cheung CY, Mao H, Lai AK, Chan RW, et al. H5N1 influenza virus-induced mediators upregulate RIG-I in uninfected cells by paracrine effects contributing to amplified cytokine cascades. J Infect Dis 2011; 204: 1866–78.
Li C, Yang P, Sun Y, Li T, Wang C, Wang Z, et al. IL-17 response mediates acute lung injury induced by the 2009 pandemic influenza A (H1N1) virus. Cell Res 2012; 22: 528–38.
Ryzhakov G, Lai CC, Blazek K, To KW, Hussell T, Udalova I . IL-17 boosts proinflammatory outcome of antiviral response in human cells. J Immunol 2011; 187: 5357–62.
Chan MC, Cheung CY, Chui WH, Tsao SW, Nicholls JM, Chan YO, et al. Proinflammatory cytokine responses induced by influenza A (H5N1) viruses in primary human alveolar and bronchial epithelial cells. Respir Res 2005; 6: 135.
Zeng H, Goldsmith C, Thawatsupha P, Chittaganpitch M, Waicharoen S, Zaki S, et al. Highly pathogenic avian influenza H5N1 viruses elicit an attenuated type I interferon response in polarized human bronchial epithelial cells. J Virol 2007; 81: 12439–49.
Friesenhagen J, Boergeling Y, Hrincius E, Ludwig S, Roth J, Viemann D . Highly pathogenic avian influenza viruses inhibit effective immune responses of human blood-derived macrophages. J Leukoc Biol 2012; 92: 11–20.
Lipatov AS, Andreansky S, Webby RJ, Hulse DJ, Rehg JE, Krauss S, et al. Pathogenesis of Hong Kong H5N1 influenza virus NS gene reassortants in mice: the role of cytokines and B- and T-cell responses. J Gen Virol 2005; 86: 1121–30.
Guan Y, Peiris JS, Lipatov AS, Ellis TM, Dyrting KC, Krauss S, et al. Emergence of multiple genotypes of H5N1 avian influenza viruses in Hong Kong SAR. Proc Natl Acad Sci U S A 2002; 99: 8950–5.
Wasilenko JL, Lee CW, Sarmento L, Spackman E, Kapczynski DR, Suarez DL, et al. NP, PB1, and PB2 viral genes contribute to altered replication of H5N1 avian influenza viruses in chickens. J Virol 2008; 82: 4544–53.
Tada T, Suzuki K, Sakurai Y, Kubo M, Okada H, Itoh T, et al. NP body domain and PB2 contribute to increased virulence of H5N1 highly pathogenic avian influenza viruses in chickens. J Virol 2011; 85: 1834–46.
Liniger M, Moulin HR, Sakoda Y, Ruggli N, Summerfield A . Highly pathogenic avian influenza virus H5N1 controls type I IFN induction in chicken macrophage HD-11 cells: a polygenic trait that involves NS1 and the polymerase complex. Virol J 2012; 9: 7.
Kajihara M, Sakoda Y, Soda K, Minari K, Okamatsu M, Takada A, et al. The PB2, PA, HA, NP, and NS genes of a highly pathogenic avian influenza virus A/whooper swan/Mongolia/3/2005 (H5N1) are responsible for pathogenicity in ducks. Virol J 2013; 10: 45.
Connor RJ, Kawaoka Y, Webster RG, Paulson JC . Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 1994; 205: 17–23.
Stevens J, Blixt O, Glaser L, Taubenberger JK, Palese P, Paulson JC, et al. Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J Mol Biol 2006; 355: 1143–55.
Ito T, Couceiro JN, Kelm S, Baum LG, Krauss S, Castrucci MR, et al. Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J Virol 1998; 72: 7367–73.
Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y . Avian flu: influenza virus receptors in the human airway. Nature 2006; 440: 435–6.
Gambaryan AS, Matrosovich TY, Philipp J, Munster VJ, Fouchier RA, Cattoli G, et al. Receptor–binding profiles of H7 subtype influenza viruses in different host species. J Virol 2012; 86: 4370–9.
Ha Y, Stevens DJ, Skehel JJ, Wiley DC . X-ray structures of H5 avian and H9 swine influenza virus hemagglutinins bound to avian and human receptor analogs. Proc Natl Acad Sci U S A 2001; 98: 11181–6.
Gamblin SJ, Haire LF, Russell RJ, Stevens DJ, Xiao B, Ha Y, et al. The structure and receptor binding properties of the 1918 influenza hemagglutinin. Science 2004; 303: 1838–42.
Xu R, McBride R, Paulson JC, Basler CF, Wilson IA . Structure, receptor binding, and antigenicity of influenza virus hemagglutinins from the 1957 H2N2 pandemic. J Virol 2010; 84: 1715–21.
Yamada S, Suzuki Y, Suzuki T, Le MQ, Nidom CA, Sakai-Tagawa Y, et al. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature 2006; 444: 378–82.
Chen LM, Blixt O, Stevens J, Lipatov AS, Davis CT, Collins BE, et al. In vitro evolution of H5N1 avian influenza virus toward human–type receptor specificity. Virology 2012; 422: 105–13.
Watanabe Y, Ibrahim MS, Ellakany HF, Kawashita N, Mizuike R, Hiramatsu H, et al. Acquisition of human-type receptor binding specificity by new H5N1 influenza virus sublineages during their emergence in birds in Egypt. PLoS Pathog 2011; 7: e1002068.
Gambaryan A, Tuzikov A, Pazynina G, Bovin N, Balish A, Klimov A . Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology 2006; 344: 432–8.
Auewarakul P, Suptawiwat O, Kongchanagul A, Sangma C, Suzuki Y, Ungchusak K, et al. An avian influenza H5N1 virus that binds to a human-type receptor. J Virol 2007; 81: 9950–5.
Belser JA, Blixt O, Chen LM, Pappas C, Maines TR, Van Hoeven N, et al. Contemporary North American influenza H7 viruses possess human receptor specificity: Implications for virus transmissibility. Proc Natl Acad Sci U S A 2008; 105: 7558–63.
Srinivasan K, Raman R, Jayaraman A, Viswanathan K, Sasisekharan R . Quantitative description of glycan-receptor binding of influenza a virus H7 hemagglutinin. PLoS One 2013; 8: e49597.
Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, et al. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 2012; 336: 1534–41.
Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, et al. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 2012; 486: 420–8.
Russell CA, Fonville JM, Brown AE, Burke DF, Smith DL, James SL, et al. The potential for respiratory droplet-transmissible A/H5N1 influenza virus to evolve in a mammalian host. Science 2012; 336: 1541–7.
Steinhauer DA . Role of hemagglutinin cleavage for the pathogenicity of influenza virus. Virology 1999; 258: 1–20.
Bottcher E, Matrosovich T, Beyerle M, Klenk HD, Garten W, Matrosovich M . Proteolytic activation of influenza viruses by serine proteases TMPRSS2 and HAT from human airway epithelium. J Virol 2006; 80: 9896–8.
Schrauwen EJ, Herfst S, Leijten LM, van Run P, Bestebroer TM, Linster M, et al. The multibasic cleavage site in H5N1 virus is critical for systemic spread along the olfactory and hematogenous routes in ferrets. J Virol 2012; 86: 3975–84.
Suguitan AL Jr, Matsuoka Y, Lau YF, Santos CP, Vogel L, Cheng LI, et al. The multibasic cleavage site of the hemagglutinin of highly pathogenic A/Vietnam/1203/2004 (H5N1) avian influenza virus acts as a virulence factor in a host-specific manner in mammals. J Virol 2012; 86: 2706–14.
Maurer-Stroh S, Lee RT, Gunalan V, Eisenhaber F . The highly pathogenic H7N3 avian influenza strain from July 2012 in Mexico acquired an extended cleavage site through recombination with host 28S rRNA. Virol J 2013; 10: 139.
Lu X, Shi Y, Gao F, Xiao H, Wang M, Qi J, et al. Insights into avian influenza virus pathogenicity: the hemagglutinin precursor HA0 of subtype H16 has an alpha-helix structure in its cleavage site with inefficient HA1/HA2 cleavage. J Virol 2012; 86: 12861–70.
Baigent SJ, McCauley JW . Glycosylation of haemagglutinin and stalk-length of neuraminidase combine to regulate the growth of avian influenza viruses in tissue culture. Virus Res 2001; 79: 177–85.
Matsuoka Y, Swayne DE, Thomas C, Rameix-Welti MA, Naffakh N, Warnes C, et al. Neuraminidase stalk length and additional glycosylation of the hemagglutinin influence the virulence of influenza H5N1 viruses for mice. J Virol 2009; 83: 4704–8.
Naffakh N, Tomoiu A, Rameix-Welti MA, van der Werf S . Host restriction of avian influenza viruses at the level of the ribonucleoproteins. Annu Rev Microbiol 2008; 62: 403–24.
Bogs J, Kalthoff D, Veits J, Pavlova S, Schwemmle M, Manz B, et al. Reversion of PB2-627E to -627K during replication of an H5N1 Clade 2.2 virus in mammalian hosts depends on the origin of the nucleoprotein. J Virol 2011; 85: 10691–8.
Shinya K, Hamm S, Hatta M, Ito H, Ito T, Kawaoka Y . PB2 amino acid at position 627 affects replicative efficiency, but not cell tropism, of Hong Kong H5N1 influenza A viruses in mice. Virology 2004; 320: 258–66.
Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, et al. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med 2013; 368: 1888–97.
Liu Q, Lu L, Sun Z, Chen GW, Wen Y, Jiang S . Genomic signature and protein sequence analysis of a novel influenza A (H7N9) virus that causes an outbreak in humans in China. Microbes Infect 2013; 15: 432–9.
Chen W, Calvo PA, Malide D, Gibbs J, Schubert U, Bacik I, et al. A novel influenza A virus mitochondrial protein that induces cell death. Nat Med 2001; 7: 1306–12.
Zell R, Krumbholz A, Eitner A, Krieg R, Halbhuber KJ, Wutzler P . Prevalence of PB1-F2 of influenza A viruses. J Gen Virol 2007; 88: 536–46.
Pasricha G, Mishra AC, Chakrabarti AK . Comprehensive global amino acid sequence analysis of PB1F2 protein of influenza A H5N1 viruses and the influenza A virus subtypes responsible for the 20th-century pandemics. Influenza Other Respi Viruses 2013; 7: 497–505.
Coleman JR . The PB1-F2 protein of influenza A virus: increasing pathogenicity by disrupting alveolar macrophages. Virol J 2007; 4: 9.
Zamarin D, Garcia-Sastre A, Xiao X, Wang R, Palese P . Influenza virus PB1-F2 protein induces cell death through mitochondrial ANT3 and VDAC1. PLoS Pathog 2005; 1: e4.
Conenello GM, Tisoncik JR, Rosenzweig E, Varga ZT, Palese P, Katze MG . A single N66S mutation in the PB1-F2 protein of influenza A virus increases virulence by inhibiting the early interferon response in vivo. J Virol 2011; 85: 652–62.
Varga ZT, Ramos I, Hai R, Schmolke M, Garcia-Sastre A, Fernandez-Sesma A, et al. The influenza virus protein PB1-F2 inhibits the induction of type I interferon at the level of the MAVS adaptor protein. PLoS Pathog 2011; 7: e1002067.
Chen CJ, Chen GW, Wang CH, Huang CH, Wang YC, Shih SR . Differential localization and function of PB1-F2 derived from different strains of influenza A virus. J Virol 2010; 84: 10051–62.
Schmolke M, Manicassamy B, Pena L, Sutton T, Hai R, Varga ZT, et al. Differential contribution of PB1-F2 to the virulence of highly pathogenic H5N1 influenza A virus in mammalian and avian species. PLoS Pathog 2011; 7: e1002186.
Garcia-Sastre A . Inhibition of interferon-mediated antiviral responses by influenza A viruses and other negative-strand RNA viruses. Virology 2001; 279: 375–84.
Hale BG, Randall RE, Ortin J, Jackson D . The multifunctional NS1 protein of influenza A viruses. J Gen Virol 2008; 89: 2359–76.
Jiao P, Tian G, Li Y, Deng G, Jiang Y, Liu C, et al. A single-amino-acid substitution in the NS1 protein changes the pathogenicity of H5N1 avian influenza viruses in mice. J Virol 2008; 82: 1146–54.
Holsinger LJ, Nichani D, Pinto LH, Lamb RA . Influenza A virus M2 ion channel protein: a structure-function analysis. J Virol 1994; 68: 1551–63.
Pinto LH, Lamb RA . The M2 proton channels of influenza A and B viruses. J Biol Chem 2006; 281: 8997–9000.
Jefferson T, Demicheli V, Di Pietrantonj C, Rivetti D . Amantadine and rimantadine for influenza A in adults. Cochrane Database Syst Rev 2006: CD 001169.
Ilyushina NA, Govorkova EA, Webster RG . Detection of amantadine-resistant variants among avian influenza viruses isolated in North America and Asia. Virology 2005; 341: 102–6.
Huang Y, Hu B, Wen X, Cao S, Xu D, Zhang X, et al. Evolution analysis of the matrix (M) protein genes of 17 H9N2 chicken influenza viruses isolated in northern China during 1998–2008. Virus Genes 2009; 38: 398–403.
CDC. Update: drug susceptibility of swine-origin influenza A (H1N1) viruses, April 2009. MMWR Morb Mortal Wkly Rep 2009; 58: 433–5.
Shiraishi K, Mitamura K, Sakai-Tagawa Y, Goto H, Sugaya N, Kawaoka Y . High frequency of resistant viruses harboring different mutations in amantadine-treated children with influenza. J Infect Dis 2003; 188: 57–61.
CDC. Fiore AE, Fry A, Shay D, Gubareva L, Bresee JS, Uyeki TM . Antiviral agents for the treatment and chemoprophylaxis of influenza — recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 2011; 60: 1–24.
WHO. Laboratory methodologies for testing the antiviral susceptibility of influenza viruses: M2 ion channel inhibitor [Updated 2013 MAY 2]. Available from: http://www.who.int/influenza/gisrs_laboratory/antiviral_susceptibility/m2inhibitor/en/index.html.
Ilyushina NA, Govorkova EA, Russell CJ, Hoffmann E, Webster RG . Contribution of H7 haemagglutinin to amantadine resistance and infectivity of influenza virus. J Gen Virol 2007; 88: 1266–74.
Stamatiou G, Foscolos GB, Fytas G, Kolocouris A, Kolocouris N, Pannecouque C, et al. Heterocyclic rimantadine analogues with antiviral activity. Bioorg Med Chem 2003; 11: 5485–92.
Zoidis G, Fytas C, Papanastasiou I, Foscolos GB, Fytas G, Padalko E, et al. Heterocyclic rimantadine analogues with antiviral activity. Bioorg Med Chem 2006; 14: 3341–8.
Ma H, Kien F, Maniere M, Zhang Y, Lagarde N, Tse KS, et al. Human annexin A6 interacts with influenza A virus protein M2 and negatively modulates infection. J Virol 2012; 86: 1789–801.
Varghese JN, Smith PW, Sollis SL, Blick TJ, Sahasrabudhe A, McKimm-Breschkin JL, et al. Drug design against a shifting target: a structural basis for resistance to inhibitors in a variant of influenza virus neuraminidase. Structure 1998; 6: 735–46.
Ison MG . Clinical use of approved influenza antivirals: therapy and prophylaxis. Influenza Other Respi Viruses 2013; 7 Suppl 1: 7–13.
Govorkova EA, Leneva IA, Goloubeva OG, Bush K, Webster RG . Comparison of efficacies of RWJ-270201, zanamivir, and oseltamivir against H5N1, H9N2, and other avian influenza viruses. Antimicrob Agents Chemother 2001; 45: 2723–32.
Yamashita M . Laninamivir and its prodrug, CS-8958: long-acting neuraminidase inhibitors for the treatment of influenza. Antivir Chem Chemother 2010; 21: 71–84.
Yamashita M, Tomozawa T, Kakuta M, Tokumitsu A, Nasu H, Kubo S . CS–8958, a prodrug of the new neuraminidase inhibitor R-125489, shows long-acting anti-influenza virus activity. Antimicrob Agents Chemother 2009; 53: 186–92.
Smith JR . Oseltamivir in human avian influenza infection. J Antimicrob Chemother 2010; 65 Suppl 2: ii25–ii33.
Ison MG . Antivirals and resistance: influenza virus. Curr Opin Virol 2011; 1: 563–73.
Ferraris O, Lina B . Mutations of neuraminidase implicated in neuraminidase inhibitors resistance. J Clin Virol 2008; 41: 13–9.
Kiso M, Ozawa M, Le MT, Imai H, Takahashi K, Kakugawa S, et al. Effect of an asparagine-to-serine mutation at position 294 in neuraminidase on the pathogenicity of highly pathogenic H5N1 influenza A virus. J Virol 2011; 85: 4667–72.
Hu Y, Lu S, Song Z, Wang W, Hao P, Li J, et al. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet 2013; 381: 2273–9.
Li X, Qi W, He J, Ning Z, Hu Y, Tian J, et al. Molecular basis of efficient replication and pathogenicity of H9N2 avian influenza viruses in mice. PLoS One 2012; 7: e40118.
Kumaki Y, Day CW, Smee DF, Morrey JD, Barnard DL . In vitro and in vivo efficacy of fluorodeoxycytidine analogs against highly pathogenic avian influenza H5N1, seasonal, and pandemic H1N1 virus infections. Antiviral Res 2011; 92: 329–40.
Furuta Y, Takahashi K, Kuno-Maekawa M, Sangawa H, Uehara S, Kozaki K, et al. Mechanism of action of T–705 against influenza virus. Antimicrob Agents Chemother 2005; 49: 981–6.
Takahashi K, Furuta Y, Fukuda Y, Kuno M, Kamiyama T, Kozaki K, et al. In vitro and in vivo activities of T-705 and oseltamivir against influenza virus. Antivir Chem Chemother 2003; 14: 235–41.
Verhelst J, Parthoens E, Schepens B, Fiers W, Saelens X . Interferon-inducible protein Mx1 inhibits influenza virus by interfering with functional viral ribonucleoprotein complex assembly. J Virol 2012; 86: 13445–55.
Li C, Ba Q, Wu A, Zhang H, Deng T, Jiang T . A peptide derived from the C-terminus of PB1 inhibits influenza virus replication by interfering with viral polymerase assembly. FEBS J 2013; 280: 1139–49.
Cheng C, Yao L, Chen A, Jia R, Huan L, Guo J, et al. Inhibitory effect of small interfering RNA specific for a novel candidate target in PB1 gene of influenza A virus. J Drug Target 2009; 17: 133–9.
Yamada K, Koyama H, Hagiwara K, Ueda A, Sasaki Y, Kanesashi SN, et al. Identification of a novel compound with antiviral activity against influenza A virus depending on PA subunit of viral RNA polymerase. Microbes Infect 2012; 14: 740–7.
Ortigoza MB, Dibben O, Maamary J, Martinez-Gil L, Leyva-Grado VH, Abreu P Jr, et al. A novel small molecule inhibitor of influenza A viruses that targets polymerase function and indirectly induces interferon. PLoS Pathog 2012; 8: e1002668.
Sidwell RW, Bailey KW, Wong MH, Barnard DL, Smee DF . In vitro and in vivo influenza virus–inhibitory effects of viramidine. Antiviral Res 2005; 68: 10–7.
Boriskin YS, Leneva IA, Pecheur EI, Polyak SJ . Arbidol: a broad-spectrum antiviral compound that blocks viral fusion. Curr Med Chem 2008; 15: 997–1005.
Kolobukhina LV, Malinovskaia VV, Gatich RZ, Merkulova LN, Burtseva EI, Isaeva EI, et al. Evaluation of the efficacy of wiferon and arbidol in adult influenza. Vopr Virusol 2008; 53: 31–3.
Fediakina IT, Leneva IA, Iamnikova SS, Livov DK, Glushkov RG, Shuster AM . [Sensitivity of influenza A/H5 viruses isolated from wild birds on the territory of Russia to arbidol in the cultured MDCK cells]. Vopr Virusol 2005; 50: 32–5.
Shumilov VI, Shuster AM, Lobastov SP, Shevtsov VA, Mednikov BL, Piiavskii SA, et al. [Efficacy of arbidol in prophylaxis and treatment of acute respiratory viral infections in servicemen]. Voen Med Zh 2002; 323: 51–3, 96.
Knight V, Gilbert BE . Ribavirin aerosol treatment of influenza. Infectious disease clinics of North America 1987; 1: 441–57.
Ilyushina NA, Hay A, Yilmaz N, Boon AC, Webster RG, Govorkova EA . Oseltamivir-ribavirin combination therapy for highly pathogenic H5N1 influenza virus infection in mice. Antimicrob Agents Chemother 2008; 52: 3889–97.
Smith CB, Charette RP, Fox JP, Cooney MK, Hall CE . Lack of effect of oral ribavirin in naturally occurring influenza A virus (H1N1) infection. J Infet Dis 1980; 141: 548–54.
Eggleston M . Clinical review of ribavirin. Infect Control 1987; 8: 215–8.
Brochot E, Francois C, Castelain S, Helle F, Van Nhien AN, Duchaussoy I, et al. A new tool to study ribavirin-induced haemolysis. Antiv Ther 2012; 17: 1311–7.
Gish RG . Treating HCV with ribavirin analogues and ribavirin–like molecules. J Antimicrob Chemother 2006; 57: 8–13.
Leneva IA, Russell RJ, Boriskin YS, Hay AJ . Characteristics of arbidol–resistant mutants of influenza virus: implications for the mechanism of anti–influenza action of arbidol. Antiviral Res 2009; 81: 132–40.
Leneva IA, Fediakina IT, Gus'kova TA, Glushkov RG . Sensitivity of various influenza virus strains to arbidol. Influence of arbidol combination with different antiviral drugs on reproduction of influenza virus A. Ter Arkh 2005; 77: 84–8.
Liu Q, Xiong HR, Lu L, Liu YY, Luo F, Hou W, et al. Antiviral and anti-inflammatory activity of arbidol hydrochloride in influenza A (H1N1) virus infection. Acta Pharmacol Sin 2013; 34: 1075–83.
Triana-Baltzer GB, Babizki M, Chan MC, Wong AC, Aschenbrenner LM, Campbell ER, et al. DAS181, a sialidase fusion protein, protects human airway epithelium against influenza virus infection: an in vitro pharmacodynamic analysis. J Antimicrob Chemother 2010; 65: 275–84.
Chan RW, Chan MC, Wong AC, Karamanska R, Dell A, Haslam SM, et al. DAS181 inhibits H5N1 influenza virus infection of human lung tissues. Antimicrob Agents Chemother 2009; 53: 3935–41.
Zhang H . DAS181 and H5N1 virus infection. J Infect Dis 2009; 199: 1250.
Belser JA, Lu X, Szretter KJ, Jin X, Aschenbrenner LM, Lee A, et al. DAS181, a novel sialidase fusion protein, protects mice from lethal avian influenza H5N1 virus infection. J Infect Dis 2007; 196: 1493–9.
Moss RB, Hansen C, Sanders RL, Hawley S, Li T, Steigbigel RT . A phase II study of DAS181, a novel host directed antiviral for the treatment of influenza infection. J Infect Dis 2012; 206: 1844–51.
Umemura M, Itoh M, Makimura Y, Yamazaki K, Umekawa M, Masui A, et al. Design of a sialylglycopolymer with a chitosan backbone having efficient inhibitory activity against influenza virus infection. J Med Chem 2008; 51: 4496–503.
Gambaryan AS, Tuzikov AB, Chinarev AA, Juneja LR, Bovin NV, Matrosovich MN . Polymeric inhibitor of influenza virus attachment protects mice from experimental influenza infection. Antiviral Res 2002; 55: 201–5.
Jones JC, Turpin EA, Bultmann H, Brandt CR, Schultz-Cherry S . Inhibition of influenza virus infection by a novel antiviral peptide that targets viral attachment to cells. J Virol 2006; 80: 11960–7.
Rajik M, Jahanshiri F, Omar AR, Ideris A, Hassan SS, Yusoff K . Identification and characterisation of a novel anti-viral peptide against avian influenza virus H9N2. Virol J 2009; 6: 74.
Li XB, Wang SQ, Xu WR, Wang RL, Chou KC . Novel inhibitor design for hemagglutinin against H1N1 influenza virus by core hopping method. PLoS One 2011; 6: e28111.
Russell RJ, Kerry PS, Stevens DJ, Steinhauer DA, Martin SR, Gamblin SJ, et al. Structure of influenza hemagglutinin in complex with an inhibitor of membrane fusion. Proc Natl Acad Sci U S A 2008; 105: 17736–41.
Wang X, Li M, Zheng H, Muster T, Palese P, Beg AA, et al. Influenza A virus NS1 protein prevents activation of NF-kappaB and induction of alpha/beta interferon. J Virol 2000; 74: 11566–73.
Droebner K, Pleschka S, Ludwig S, Planz O . Antiviral activity of the MEK-inhibitor U0126 against pandemic H1N1v and highly pathogenic avian influenza virus in vitro and in vivo. Antiviral Res 2011; 92: 195–203.
Ludwig S . Targeting cell signalling pathways to fight the flu: towards a paradigm change in anti-influenza therapy. J Antimicrob Chemother 2009; 64: 1–4.
Mazur I, Wurzer WJ, Ehrhardt C, Pleschka S, Puthavathana P, Silberzahn T, et al. Acetylsalicylic acid (ASA) blocks influenza virus propagation via its NF-kappaB-inhibiting activity. Cell Microbiol 2007; 9: 1683–94.
Brett SJ, Myles P, Lim WS, Enstone JE, Bannister B, Semple MG, et al. Pre-Admission Statin Use and In-Hospital Severity of 2009 Pandemic Influenza A (H1N1) Disease. PloS one 2011; 6.
Viasus D, Pano-Pardo JR, Cordero E, Campins A, Lopez-Medrano F, Villoslada A, et al. Effect of immunomodulatory therapies in patients with pandemic influenza A (H1N1) 2009 complicated by pneumonia. J Infect 2011; 62: 193–9.
Barik S . New treatments for influenza. BMC Med 2012; 10: 104.
Walsh KB, Teijaro JR, Wilker PR, Jatzek A, Fremgen DM, Das SC, et al. Suppression of cytokine storm with a sphingosine analog provides protection against pathogenic influenza virus. Proc Natl Acad Sci U S A 2011; 108: 12018–23.
Marsolais D, Hahm B, Walsh KB, Edelmann KH, McGavern D, Hatta Y, et al. A critical role for the sphingosine analog AAL-R in dampening the cytokine response during influenza virus infection. Proc Natl Acad Sci U S A 2009; 106: 1560–5.
MOH of PR China. Guidelines for Management of Pandemic (H1N1) 2009 Influenza [updated 2013 May 2]. Available from: http://www.moh.gov.cn/mohwsyjbgs/s9990/200910/43111.shtml.
MOH of PR China. Guidelines for Management of Avian H7N9 Influenza Infection [updated 2013 May 2]. Available from: http://www.moh.gov.cn/ewebeditor/uploadfile/2013/04/20130410212136993.doc.
Chen X, Wu T, Liu G . Chinese medicinal herbs for influenza: a systematic review. J Altern Complement Med 2006; 12: 171–80.
Chen W, Lim CE, Kang HJ, Liu J . Chinese herbal medicines for the treatment of type A H1N1 influenza: a systematic review of randomized controlled trials. PloS One 2011; 6: e28093.
Poon PM, Wong CK, Fung KP, Fong CY, Wong EL, Lau JT, et al. Immunomodulatory effects of a traditional Chinese medicine with potential antiviral activity: a self-control study. The Am J Chin Med 2006; 34: 13–21.
Bottcher-Friebertshauser E, Freuer C, Sielaff F, Schmidt S, Eickmann M, Uhlendorff J, et al. Cleavage of influenza virus hemagglutinin by airway proteases TMPRSS2 and HAT differs in subcellular localization and susceptibility to protease inhibitors. J Virol 2010; 84: 5605–14.
Bottcher-Friebertshauser E, Lu Y, Meyer D, Sielaff F, Steinmetzer T, Klenk HD, et al. Hemagglutinin activating host cell proteases provide promising drug targets for the treatment of influenza A and B virus infections. Vaccine 2012; 30: 7374–80.
Zhirnov OP, Klenk HD, Wright PF . Aprotinin and similar protease inhibitors as drugs against influenza. Antiviral Res 2011; 92: 27–36.
Walkiewicz MP, Basu D, Jablonski JJ, Geysen HM, Engel DA . Novel inhibitor of influenza non-structural protein 1 blocks multi-cycle replication in an RNase L-dependent manner. J Gen Virol 2011; 92: 60–70.
Nacken W, Ehrhardt C, Ludwig S . Small molecule inhibitors of the c-Jun N-terminal kinase (JNK) possess antiviral activity against highly pathogenic avian and human pandemic influenza A viruses. Biol Chem 2012; 393: 525–34.
Acknowledgements
The research on arbidol was supported by the National Mega Project on Major Drug Development (2009ZX 09301-014-1).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Liu, Q., Liu, Dy. & Yang, Zq. Characteristics of human infection with avian influenza viruses and development of new antiviral agents. Acta Pharmacol Sin 34, 1257–1269 (2013). https://doi.org/10.1038/aps.2013.121
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2013.121
Keywords
This article is cited by
-
Profiling the TRB and IGH repertoire of patients with H5N6 Avian Influenza Virus Infection by high-throughput sequencing
Scientific Reports (2019)
-
The Establishment and Validation of the Human U937 Cell Line as a Cellular Model to Screen Immunomodulatory Agents Regulating Cytokine Release Induced by Influenza Virus Infection
Virologica Sinica (2019)
-
Serological evidence of H9N2 avian influenza virus exposure among poultry workers from Fars province of Iran
Virology Journal (2016)
-
The cytokine storm of severe influenza and development of immunomodulatory therapy
Cellular & Molecular Immunology (2016)
-
Visualizing real-time influenza virus infection, transmission and protection in ferrets
Nature Communications (2015)