Abstract
Drug discovery and development is a complex, high risk, time consuming and potentially highly rewarding process. Pharmaceutical companies literally burn millions of dollar per drug to bring it to the market. The development of a new drug requires a technological expertise, human resources and huge capital investment. It also requires strict adherence to regulations on testing and manufacturing standards before a new drug comes into market and can be used in the general population, in fact, some time it fails to come into market. All these factors just increase the cost for a new chemical entity research and development. Two branches which made positive impact on drug designing process and reduce the overall cost and risk are Bioinformatics and Pharmacogenomics. Their practice in drug designing process made positive effect on overall process and they can accelerate various steps of drug designing, and reduce the cost and over all time. Current note focusses on the role of bioinformatics and pharmacogenomics in drug discovery and development process.
Similar content being viewed by others
1 Bioinformatics and drug discovery
Drug discovery is the step-by-step process by which new candidate drugs are discovered. Traditionally, pharmaceutical companies follow well-established pharmacology and chemistry-based drug discovery approaches, and face various difficulties in finding new drugs (Iskar et al. 2012). In the highly competitive “winner takes all” pharmaceutical industry, the first company to patent a new chemical entity (NCE i.e., new drug candidate) for a specific treatment takes all the spoils, leaving other competitors to mostly wait for patent expirations to partake in the largesse (Iskar et al. 2012). Nowadays, therefore, Pharmaceutical companies invest heavily in all those approaches that show potential to accelerate any phase of the drug development process (Whittaker 2003). The increasing pressure to generate more and more drugs in a short period of time with low risk has resulted in remarkable interest in bioinformatics (Ortega et al. 2012). In fact, now there is an existence of new, separate field, known as computer-aided drug design (CADD), (Song et al. 2009; Speck-Planche and Cordeiro 2013).
1.1 Drug target identification
One of the major thrusts of current bioinformatics approaches is the prediction and identification of biologically active candidates (Whittaker 2003), and mining and storage of related information (Table 1). Drugs are usually only developed when the particular drug target for those drugs’ actions have been identified and studied. The number of potential targets for drug discovery process is increasing exponentially. Mining and warehousing of the human genome sequence using bioinformatics has helped to define and classify the nucleotide compositions of those genes, which are responsible for the coding of target proteins, in addition to identifying new targets that offer more potential for new drugs (Chen and Chen 2008; Katara et al. 2011). This is an area where the human genome information is expected to play a master role (Yamanishi et al. 2010). Drug developers are presented with an unaccustomed luxury of choice as more genes are identified and the drug discovery cycle becomes more data-intensive (Loh and Soong 2011). Bioinformatics allows the identification and analysis of more and more biological drug targets; thus expected to greatly increase the breath of potential drugs in the pipelines of pharmaceutical companies (Whittaker 2003; Ortega et al. 2012).
1.2 Drug target validation
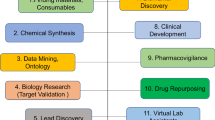
Bioinformatics also provides strategies and algorithm to predict new drug targets and to store and manage available drug target information. After the discovery of “potential” drug targets, there is an inappreciable need to establish a strong association between a putative target and disease of interest (Yamanishi et al. 2010). The establishment of such a key association provides justification for the drug development process. This process, known as target validation, is an area where bioinformatics is playing a significant role (Fig. 1). Drug target validation helps to moderate the potential for failure in the clinical testing and approval phases (Ratti and Trist 2001; Gilbert et al. 2003; Whittaker 2003).
1.3 Cost reduction
The current high cost of drug discovery and development is a major cause for concern among pharmaceutical companies (Dickson and Gagnon 2004a, b; Adams and Brantner 2010). Along with increasing productivity, pharmaceutical companies also aim to reduce the high failure rate in the drug discovery process so that increased number of drugs able to hit the market (Tsaioun et al. 2009). The high cost of various phase of clinical trials acts as limiting factors for number of drugs, which can be developed by pharmaceutical companies, and hence selecting the compounds with the best chances for approval is critical (Klein and Tabarrok 2003; Wierenga and Eaton 2004; Tamimi and Ellis 2009). The costs of drug discovery and development—generally include total costs from discovery to approval (Klein and Tabarrok 2003; Wierenga and Eaton 2004; Adams and Brantner 2010) though some studies have included the costs of failed drugs and the costs for commercialization (Gilbert et al. 2003). There is also a cost associated with the elongated process, beginning from discovery all the way to final approval (Klein and Tabarrok 2003; Tamimi and Ellis 2009). Advances in bioinformatics accelerate drug discovery process, beginning with drug target identification and validation (viz., Docking), to assay development, and virtual-high-throughput screening (v-HTS)—all with the goal of identifying new potential chemical entities.
Bioinformatics provides more efficient target discovery and validation approaches, thus help to ensure that more drug candidates are successful during the approval process and making it more cost-effective (Ortega et al. 2012).
1.4 Promote novel/new drug development
There are some collateral costs that bother the pharmaceutical industry (Collier 2009). These costs include commercialization costs (Gilbert et al. 2003; Mullin 2003; Liang and Mackey 2011), litigation and drug-recall costs (Klein and Tabarrok 2003), and general costs to society (Lazarou et al. 1998; Rawlins 2004). Commercialization costs for new drug to be about $250 million per approved drugs (Gilbert et al. 2003; Dickson and Gagnon 2004a, b), are high mainly because most “new” drugs approved are essentially functional replicas of drugs that already exist. Most of the copycat drugs are being commercialized to handle the illness for which there are drugs already; thus, there is a need of interface that can attract the attention of both physicians and patients who already have access to similar medication (Meyers and Baker 2001). Bioinformatics can act as proper interface, and provides new approaches and opportunities to pharmaceutical companies to efficiently discover potential drug targets and develop novel drugs (Whittaker 2003). If drugs are not commercialized in competition with already existing equivalents, their commercialization costs are expected to fall significantly (Meyers and Baker 2001; Simoens 2011; Liang and Mackey 2011).
1.5 Barriers to bioinformatics progress in drug design process
Bioinformatics efforts did not make any impeccable changes in the drug discovery and development process. This may be because the practice of bioinformatics is relatively new and has only attained prominence in the years following the partial completion of the Human Genome Project (Lindpaintner 2002). Till now, bioinformatics has not made any considerable impact, as projected earlier, on the cost of drugs. The pharmaceutical industry continues to witness rising costs and withdrawals of drugs from the market after they had been approved and commercialized—because of multiple documented cases of adverse drug reactions (Shin 2012).
It has been observed that several pharmaceutical industries are facing drug discovery and development-related challenges. These challenges range from high cost of drug discovery to the lengthy and risky trials and approval process, and some time, withdrawal of previously approved drugs from the market and the innovation gap resulting from the dogged quest for blockbuster drugs (Papanikolaw 1999; Gilbert et al. 2003; Klein and Tabarrok 2003; Iskar et al. 2012). Bioinformatics was widely projected to strengthen the identification of drug targets (Zemlo 2004; Katara et al. 2011). The fact that these problems remain mostly unsolved, despite significant bioinformatics investments, is an indication of a larger problem (Blundell et al. 2006; Dhaliwal and Chen 2009; Du and Huang 2012).
2 Pharmacogenomics in drug discovery and development
Pharmacogenomics refers to the effects of genetic polymorphism and genomic variants on drug response, its knowledge can help in selection of the optimal drug, dose, and treatment process and avoid adverse drug reactions (Amstutz and Carleton 2011). The knowledge of disease-linked genetic biomarkers guides pharmaceutical companies to design pharmacogenomics-based, more précised and individualized drug and dosages (Liou et al. 2012). This is accomplished by observing genetic patterns and polymorphism of those genetic elements, which show interaction with drugs or its by-products and somehow relate with drugs pharmacokinetics of pharmacodynamics (Bernard 2003; Whittaker 2003; Liou et al. 2012).
Adverse drug reactions have been reported as one of the leading causes of death among hospitalized patients, contributing the majority of the $17 to $29 billion annual costs of medical errors (Lazarou et al. 1998; Rawlins 2004; Prows and Prows 2004). Adverse drug reactions are also reported as the factor behind loss of confidence in the healthcare system and the diminishing satisfaction of both patients and health professionals (Becquemont 2009).
2.1 Personalized/effective medication
Pharmacogenomics approach enables pharmaceutical companies to design drugs that satisfied the requirements of particular genetic sub-groups of the general population (Nelson et al. 2009). The main interest of pharmacogenomics is to identify patients for whom drug efficacy can be predicted, and to reduce risk of adverse drugs effects (Nelson et al. 2009). The promise of pharmacogenomic approaches to prescribe drugs on the basis of their patients’ genetic profiles is termed as ‘Personalized medicine’. This would reduce the speculation in drug prescriptions and thus increase the confidence of both physician and patient, and modify the predominating approaches to drug discovery and development, diagnostics, therapies and disease prevention strategies (Prows and Prows 2004; Zemlo 2004). There is also a benefit to society as the use of expensive drugs is avoided in patients whose disorders would not have been cured by these drugs (Gomase et al. 2008; Nelson et al. 2009). Bioinformatics also provides the pharmacogenomics-related information resources (Thorn et al. 2010), which contains information about the different types of polymorphism (i.e., SNP in CYP family genes) and resulted variable drug response (Table 2).
Various drugs are reported to show adverse drug reactions (ADR), which often result in hospitalizations and in some cases fatalities (Lazarou et al. 1998; Rawlins 2004; Prows and Prows 2004). The investigations of such lethal drug reaction are resulting in the withdrawal of the culprit drug from the market (Bernard 2003). This is immediately followed by a series of lawsuits and grievance for pharmaceutical malpractice. A pharmacogenomic approach for drug development strategy presents an opportunity to reverse this trend. The promise of pharmacogenomics may lead to the “development of personalized precision-pharmaceuticals”. Personalized precision-pharmaceuticals refer to drugs (and dosages of these drugs) that are tailored to an individual’s genetic composition (Bernard 2003; Zemlo 2004). These précised drugs can be evaluated in short and simplified clinical trials and will show little or no adverse effects (Zemlo 2004). Genetic verification and testing prior to drug prescription greatly reduce the chances for wrong prescriptions (Bernard 2003; Crews et al. 2012).
2.2 Revive orphan drug
In the process of drug discovery and development, pharmaceutical companies stay mostly focused on the major drugs that are prescribed to upwards of 20 million people, such drugs are known as Blockbuster drugs. The result of this is a loss of drug that may have been developed to cure diseases that affect only a small number of people (Klein and Tabarrok 2003). These drugs—or potential drugs are known as abandoned or orphaned drugs (Klein and Tabarrok 2003). A pharmacogenomic strategy to drug development may revive these orphaned drugs if it can be demonstrated that there are potential beneficiaries for these drugs (Bernard 2003; Maher and Haffner 2006; Simoens 2011). From a business point of view, if the pharmaceutical company could benefit from something like orphan drug status for its product, this would help encourage stratification of populations on the basis of pharmacogenomics, since the reduction in the size of a population to be treated could be compensated by preference for the drug. This is the only way that pharmaceutical companies can be encouraged to give up the blockbuster dogma (Nelson et al. 2009; Simoens 2011).
In recent years, various International food and drug authorities have recognized the potential of pharmacogenomics and encouraged such approaches to drug discovery and delivery process (Rioux 2000; Liou et al. 2012). As pharmacogenomic technologies continue to emerge and mature, the international regulatory bodies develop pharmacogenomic guidelines and regulations. Nevertheless, the increased attention and the documented potential and promise of pharmacogenomics-based drug development strategies, there has been continuous resistance to this approach on the part of pharmaceutical companies (Bernard 2003; Liou et al. 2012). The reason behind such resistance is the perception that a pharmacogenomics strategy will lead to a significant loss of revenue resulting from the fragmentation of the drug market. Alongside, such perception is ejected and just considered as ‘myth’ by some workers, they reported that a pharmacogenomic strategy has the potential to increase drug market size, depending on variety of factors (Bernard 2003).
2.3 Barriers to pharmacogenomics progress in drug designing and development
Pharmacogenomics is based on genomic variations specifically in coding or near to coding regions. It is very difficult to predict gene variations that affect drug response. Single nucleotide polymorphisms (SNPs) play a major role in variable drug response. SNPs occur every 100–300 bases along the three-billion-base human genome; therefore, millions of SNPs must be identified and analyzed to determine their involvement (if any) in drug response (Laing et al. 2011). Limited awareness and knowledge toward the relationship between gene variants and variable drug response also act as limiting factor to implicate pharmacogenomics-based drug design and delivery process. Since many genes are likely to influence responses, obtaining the big picture on the impact of gene variations is highly time consuming and complicated, and for such purpose, we need genetic profile of each individual, which not seems possible in near future (Vanakker and De Paepe 2013). Doctors also need to execute an extra diagnostic step to determine which drug is best suited to each patient. To interpret the diagnostic accurately and recommend the best course of treatment for each patient, all prescribing physicians, regardless of specialty, will need a better understanding of genetics (Ginsburg and Willard 2009; Becquemont et al. 2011). Several ethical considerations also need to be made prior to routine clinical implementation of pharmacogenomics (Haga and Burke 2011). At the same time, the economics of pharmacogenomic testing from the perspective of patients, clinicians, insurance companies, governments, and pharmaceutical companies will play an important role in determining its future use.
3 Conclusions
Drug designing is a very complex, expensive and time consuming process. Both Bioinformatics and Pharmacogenomics provide a huge support to overcome the cost and time context in various ways. Bioinformatics provides wide range of drug-related databases and softwares, which can be used for various purposes, related to drug designing and development process. Likewise, pharmacogenomics provides the genome level information about the variable drug response, which is very important for pharmaceutical companies to design new drug, along with orphan drug, and save already existing drugs. Though, bioinformatics and pharmacogenomics are still in their initial phase and presently facing some hurdles, they show enough potential to help drug development process in near future.
References
Adams CP, Brantner VV (2010) Spending on new drug development. Health Econ 19:130–141
Amstutz U, Carleton BC (2011) Pharmacogenetic testing: time for clinical practice guidelines. Clin Pharmacol Ther 89:924–927
Becquemont L (2009) Pharmacogenomics of adverse drug reactions: practical applications and perspectives. Pharmacogenomics 10:961–969
Becquemont L, Alfirevic A, Amstutz U, Brauch H, Jacqz-Aigrain E, Laurent-Puig P, Molina MA, Niemi M, Schwab M, Somogyi AA, Thervet E, Maitland-van der Zee AH, van Kuilenburg AB, van Schaik RH, Verstuyft C, Wadelius M, Daly AK (2011) Practical recommendations for pharmacogenomics-based prescription: 2010 ESF-UB Conference on Pharmacogenetics and Pharmacogenomics. Pharmacogenomics 12:113–124
Bernard S (2003) The 5 Myths of Pharmacogenomics. Pharm Executive 23:70–78
Blundell TL, Sibanda BL, Montalvao RW, Brewerton S, Chelliah V, Worth CL, Harmer NJ, Davies O, Burke D (2006) Structural biology and bioinformatics in drug design: opportunities and challenges for target identification and lead discovery. Philos Trans R Soc Lond B Biol Sci 361:413–423
Chen YP, Chen F (2008) Identifying targets for drug discovery using bioinformatics. Expert Opin Ther Targ 12:383–389
Collier R (2009) Rapidly rising clinical trial costs worry researchers. CMAJ 180:277–278
Crews KR, Hicks JK, Pui CH, Relling MV, Evans WE (2012) Pharmacogenomics and individualized medicine: translating science into practice. Clin Pharmacol Ther 92:467–475
Dhaliwal B, Chen YW (2009) Computational resources for protein modelling and drug discovery applications. Infect Disord Drug Targ 9:557–562
Dickson M, Gagnon JP (2004a) Key factors in the rising cost of new drug discovery and development. Nat Rev Drug Discov 3:417–429
Dickson M, Gagnon JP (2004b) The cost of new drug discovery and development. Discov Med 4:172–179
Du QS, Huang RB (2012) Recent progress in computational approaches to studying the M2 proton channel and its implication to drug design against influenza viruses. Curr Protein Pept Sci 13:205–210
Gilbert J, Henske P, Singh A (2003) Rebuilding Big Pharma’s Business Model. In vivo Business and Medicine Report 21, p 10
Ginsburg GS, Willard HF (2009) Genomic and personalized medicine: foundations and applications. Transl Res 154:277–287
Gomase VS, Tagore S, Changbhale SS, Kale KV (2008) Pharmacogenomics. Curr Drug Metab 9:207–212
Haga SB, Burke W (2011) Practical ethics: establishing a pathway to benefit for complex pharmacogenomic tests. Clin Pharmacol Ther 90:25–27
Hecker N, Ahmed J, von Eichborn J, Dunkel M, Macha K, Eckert A, Gilson MK, Bourne PE, Preissner R (2012) Super target goes quantitative: update on drug-target interactions. Nucleic Acids Res 40:D1113–D1117
Iskar M, Zeller G, Zhao XM, van Noort V, Bork P (2012) Drug discovery in the age of systems biology: the rise of computational approaches for data integration. Curr Opin Biotechnol 23:609–616
Katara P, Grover A, Kuntal H, Sharma V (2011) In silico prediction of drug targets in vibrio cholerae. Protoplasma 248:799–804
Klein DB, Tabarrok A (2003) The drug discovery, development and approval process. www.fdareview.org
Kuhn M, Szklarczyk D, Franceschini A, Campillos M, von Mering C, Jensen LJ, Beyer A, Bork P (2010) STITCH 2: an interaction network database for small molecules and proteins. Nucleic Acids Res 38:D552–D556
Laing RE, Hess P, Shen Y, Wang J, Hu SX (2011) The role and impact of SNPs in pharmacogenomics and personalized medicine. Curr Drug Metab 12:460–486
Lazarou J, Pomeranz BH, Corey PN (1998) Incidence of adverse drug reactions in hospitalized patients. JAMA 279:1200–1205
Liang BA, Mackey T (2011) Direct-to-consumer advertising with interactive internet media: global regulation and public health issues. JAMA 305:824–825
Lindpaintner K (2002) The impact of pharmacogenetics and pharmacogenomics on drug discovery. Nat Rev Drug Discov 1:463–469
Liou SY, Stringer F, Hirayama M (2012) The impact of pharmacogenomics research on drug development. Drug Metab Pharmacokinet 27:2–8
Loh M, Soong R (2011) Challenges and pitfalls in the introduction of pharmacogenetics for cancer. Ann Acad Med Singap 40:369–374
Maher PD, Haffner M (2006) Orphan drug designation and pharmacogenomics: options and opportunities. BioDrugs 20:71–79
Meyers S, Baker A (2001) Drug discovery: an operating model for a new era. Nat Biotechnol 19:727–730
Mullin R (2003) Drug Development Costs About $1.7 Billion. Chemical and Engineering News April 2003
Nelson MR, Bacanu SA, Mosteller M, Li L, Bowman CE, Roses AD, Lai EH, Ehm MG (2009) Genome-wide approaches to identify pharmacogenetic contributions to adverse drug reactions. Pharmacogenomics J 9:23–33
Ortega SS, Cara LC, Salvador MK (2012) In silico pharmacology for a multidisciplinary drug discovery process. Drug Metabol Drug Interact 27:199–207
Papanikolaw J (1999) Bioinformatics emerges as key technology for developing new drugs. Chem Mark Report 21:22
Prows CA, Prows DR (2004) Medication selection by genotype: how genetics is changing drug prescription and efficacy. Am J Nurs 104:60–70
Ratti E, Trist D (2001) Continuing evolution of the drug discovery process. Pure Appl Chem 73:67–75
Rawlins MD (2004) Cutting the cost of drug development? Nat Rev Drug Discov 3:360–364
Rioux PP (2000) Clinical trials in pharmacogenetics and pharmacogenomics: methods and applications. Am J Health Syst Pharm 57:887–901
Scherf U, Becker R, Chan M, Hojvat S (2010) Approval of novel biomarkers: fDA’s perspective and major requests. Scand J Clin Lab Invest Suppl 242:96–102
Sherry ST, Ward MH, Kholodov M, Baker J, Phan L, Smigielski EM, Sirotkin K (2001) dbSNP: the NCBI database of genetic variation. Nucleic Acids Res 29:308–311
Shin J (2012) Clinical pharmacogenomics of warfarin and clopidogrel. J Pharm Pract 25:428–438
Sim SC, Ingelman-Sundberg M (2010) The human cytochrome P450 (CYP) allele nomenclature website: a peer-reviewed database of CYP variants and their associated effects. Hum Genomics 4:278–281
Simoens S (2011) Pricing and reimbursement of orphan drugs: the need for more transparency. Orphanet J Rare Dis 6:42
Song CM, Lim SJ, Tong JC (2009) Recent advances in computer-aided drug design. Brief Bioinform 10:579–591
Speck-Planche A, Cordeiro MN (2013) Computer-aided drug design, synthesis and evaluation of new anti-cancer drugs. Curr Top Med Chem [Epub ahead of print]
Tamimi NA, Ellis P (2009) Drug development: from concept to marketing! Nephron Clin Pract 113:c125–c131
Thorisson GA, Smith AV, Krishnan L, Stein LD (2005) The international HapMap project web site. Genome Res 15:1592–1593
Thorn CF, Klein TE, Altman RB (2010) Pharmacogenomics and bioinformatics: pharmGKB. Pharmacogenomics 11:501–505
Tsaioun K, Bottlaender M, Mabondzo A, Alzheimer’s Drug Discovery Foundation (2009) ADDME–avoiding drug development mistakes early: central nervous system drug discovery perspective. BMC Neurol 12:9
Vanakker OM, De Paepe A (2013) Pharmacogenomics in children: advantages and challenges of next generation sequencing applications. Int J Pediatr 2013:136524
Whittaker P (2003) What is the relevance of bioinformatics to pharmacology? Trend Pharmacol Sci 24:434–439
Wierenga DE, Eaton RC (2004) Drug Development and Approval Process. Alliance Pharmaceutical Company. http://www.allp.com/drug_dev.htm
Wishart DS, Knox C, Guo AC, Cheng D, Shrivastava S, Tzur D, Gautam B, Hassanali M (2008) DrugBank: a knowledgebase for drugs, drug actions and drug targets. Nucleic Acids Res 36:D901–D906
Yamanishi Y, Kotera M, Kanehisa M, Goto S (2010) Drug-target interaction prediction from chemical, genomic and pharmacological data in an integrated framework. Bioinformatics 26:i246–i254
Zemlo T (2004) Pharmacogenomic promise, pitfalls. Drug discovery and development. Highland Ranch 7:13
Zhu F, Shi Z, Qin C, Tao L, Liu X, Xu F, Zhang L, Song Y, Liu X, Zhang J, Han B, Zhang P, Chen Y (2012) Therapeutic target database update 2012: a resource for facilitating target-oriented drug discovery. Nucleic Acids Res 40:D1128–D1136
Acknowledgments
Authors acknowledge the Department of Bioscience and Biotechnology, Banasthali University, Banasthali, India for their support.
Conflict of interest
No competing financial interests exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Katara, P. Role of bioinformatics and pharmacogenomics in drug discovery and development process. Netw Model Anal Health Inform Bioinforma 2, 225–230 (2013). https://doi.org/10.1007/s13721-013-0039-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13721-013-0039-5